Tuberculous lymphadenitis
| Tuberculous lymphadenitis | |
|---|---|
| Other names: Tuberculous adenitis[1] | |
  | |
| |
| Specialty | Infectious disease |
| Symptoms | Enlarged lymph nodes,fever, night sweats[2] |
| Causes | TB[2] |
| Diagnostic method | Biopsy, Acid-fast stain test[3] |
| Differential diagnosis | Fungal infections, viral infections[4] |
| Treatment | Isoniazid, rifampin, pyrazinamide[5][6] |
Tuberculous lymphadenitis (or tuberculous adenitis) is the most common form of tuberculosis infections that appears outside the lungs. Tuberculous lymphadenitis is a chronic, specific granulomatous inflammation of the lymph node with caseation necrosis, caused by infection with Mycobacterium tuberculosis or related bacteria.[7][2]
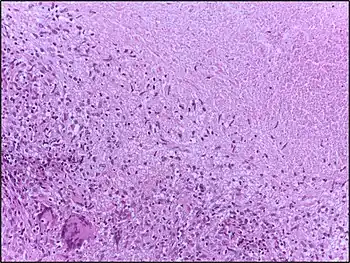
The characteristic morphological element is the tuberculous granuloma (caseating tubercule). This consists of giant multinucleated cells and (Langhans cells), surrounded by epithelioid cells aggregates, T cell lymphocytes and fibroblasts. Granulomatous tubercules eventually develop central caseous necrosis and tend to become confluent, replacing the lymphoid tissue.[8][9]
Treatment with anti-tubercular medications can lasts up to one year.[2]
Symptoms and signs
In addition to swollen lymph nodes, called lymphadenitis, the person may experience mild fevers, not feel like eating, or lose weight.[2]
Complications
In terms of complications an individual with Tuberculosis lymphadenitis may have:[10]
- Scarring
- Recurrence
- Hoarseness(enlarged lymph nodes compression)
Cause
It is usually caused by the most common cause of tuberculosis in the lungs, namely Mycobacterium tuberculosis.[2] It has sometimes also been caused by related bacteria, including M. bovis, M. kansasii, M. fortuitum, M. marinum, and Mycobacterium ulcerans.[2]
Mechanism
In terms of the disease pathophysiology we find it begins when the bacteria are carried by immune cells to lymph nodes, after inhalation into the lungs. The body's immune system forms a granuloma to contain the infection. The granuloma is characterized by central area of caseous necrosis surrounded by a ring of specialized immune cells. As the infection progresses these granulomas grow and coalesce, leading to significant enlargement of the lymph nodes(lymphadenopathy) and the formation of cold abscess, which can rupture through the skin as a sinus tract[11][6]
Diagnosis
The diagnosis of tuberculous lymphadenitis may require a biopsy. Other possible diagnostic steps include: positive tuberculin test, chest radiograph, CT scan, cytology/biopsy (FNAC), AFB staining, and mycobacterial culture.[3][6]
-
![Diagnostic algorithm of chronic lymphadenopathy[12]](./_assets_/ba48700f93e6ccab7a94adacb8f4c793/Fpubh-04-00031-g001.jpg) Diagnostic algorithm of chronic lymphadenopathy[12]
Diagnostic algorithm of chronic lymphadenopathy[12] -
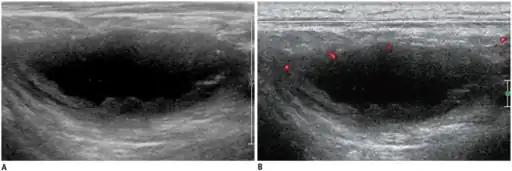 a,b)Individual diagnosed with tuberculous lymphadenitis -ultrasonography/Doppler ultrasonography
a,b)Individual diagnosed with tuberculous lymphadenitis -ultrasonography/Doppler ultrasonography
Stages
Tuberculous lymphadenitis is popularly known as collar stud abscess, due to its proximity to the collar bone and its superficial resemblance to a collar stud, although this is just one of the five stages of the disease. One or more affected lymph nodes can also be in a different body part, although it is most typical to have at least one near the collar bone.The characteristic morphological element is the tuberculous granuloma (caseating tubercule): giant multinucleated cells (Langhans cells), surrounded by epithelioid cells aggregates, T cell lymphocytes and few fibroblasts. Granulomatous tubercules evolve to central caseous necrosis and tend to become confluent, replacing the lymphoid tissue.[13][14]
Stages of tubercular lymphadenitis:[15]
- Lymphadenitis
- Periadenitis
- Cold abscess
- 'Collar stud' abscess
- Sinus
_lymph_node_biopsy.jpg)
Differential diagnosis
As to the DDx of Tuberculosis lymphadenitis we find the following:[4]
- Fungal infections
- Viral infections
- Malignancies
- Non-infectious granulomatous diseases
Treatment
Treatment with anti-tubercular medications normally lasts up to one year.[2] Symptoms may temporarily get worse during treatment.[14]Antibiotic therapy with multiple drugs, such as isoniazid, rifampin, pyrazinamide, and ethambutol[6][5]
Surgery may be required in some cases to remove infected lymph nodes[4]
Prognosis
As to prognosis we find that a high cure rate is evident; most individuals respond well to standard anti-tuberculosis therapy[16]
Epidemiology
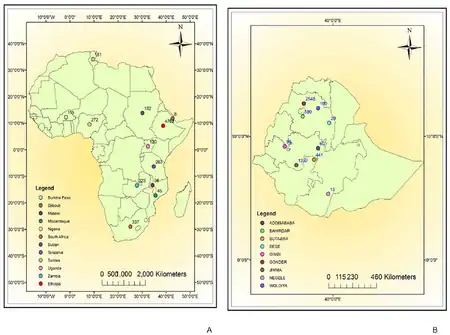
Tuberculous lymphadenitis is seen in most developing countries, especially in the context of HIV/AIDS.[2]
It is the most common extrapulmonary TB; TBL accounts for a large proportion of extrapulmonary TB cases worldwide. In some countries, it can make up 20 percent or more of all TB cases, and in countries with high TB and HIV burdens, this number can be even higher[17]
TBL is prevalent in countries where TB is endemic, particularly in Asia and Africa. India, Indonesia, and China have the highest numbers of new TB cases globally[18]
History
As to history in the 19th century, scientists began to understand the true nature of this disease. In the mid-to-late 1800s Bollinger, May, and Demme noted a microbiological connection, linking scrofula to Mycobacterium bovis from cows.[16]In 1882 Robert Koch identified Mycobacterium tuberculosis as the bacillus responsible for tuberculosis[19]
Research
As for recent studies have explored better ways to diagnose Tuberculous lymphadenitis using new antigen detection tests. These tests focus on the M. tuberculosis complex-specific antigen MPT64 and have demonstrated improved diagnostic accuracy compared to traditional methods[20]
See also
References
- ↑ De Backer, A. I.; Mortelé, K. J.; Van Den Heuvel, E.; Vanschoubroeck, I. J.; Kockx, M. M.; Van de Vyvere, M. (1 April 2007). "Tuberculous adenitis: comparison of CT and MRI findings with histopathological features". European Radiology. 17 (4): 1111–1117. doi:10.1007/s00330-006-0412-1. ISSN 1432-1084. PMID 17180329.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 M, Sriram Bhat (2016-06-30). SRB's Manual of Surgery. JP Medical Ltd. pp. 55–56. ISBN 9789351524168. Archived from the original on 2023-02-02. Retrieved 2023-01-03.
- ↑ 3.0 3.1 Mohapatra, PR; Janmeja, AK (August 2009). "Tuberculous lymphadenitis". The Journal of the Association of Physicians of India. 57: 585–90. ISSN 0004-5772. PMID 20209720.subscription required
- ↑ 4.0 4.1 4.2 Deveci, Hande Senem; Kule, Mustafa; Kule, Zeynep Altin; Habesoglu, Tulay Erden (2016). "Diagnostic challenges in cervical tuberculous lymphadenitis: A review". Northern Clinics of Istanbul. 3 (2): 150–155. doi:10.14744/nci.2016.20982. ISSN 2536-4553. PMC 5206468. PMID 28058405.
- ↑ 5.0 5.1 "WHO consolidated guidelines on tuberculosis: module 4: treatment and care". www.who.int. Archived from the original on 9 August 2025. Retrieved 26 September 2025.
- ↑ 6.0 6.1 6.2 6.3 "Scrofula: Practice Essentials, Pathophysiology of Scrofula, Epidemiology of Scrofula". eMedicine. 28 March 2025. Retrieved 23 September 2025.
- ↑ Bennett, John E.; Dolin, Raphael; Blaser, Martin J.; Mandell, Gerald L. (19 October 2009). Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases E-Book. Elsevier Health Sciences. p. 3158. ISBN 978-1-4377-2060-0. Retrieved 26 September 2025.
- ↑ Purbaningsih, Wida; Rachmawati, Meike; Triyani, Yani; Rahmi, Fadhilat Sabila (21 December 2023). "Histopathological Review of Granuloma in Diagnosis of Tuberculosis Lymphadenitis (TBL)". Global Medical & Health Communication (GMHC). 11 (3). doi:10.29313/gmhc.v11i3.12742.
- ↑ Atnafu, Abay; Wassie, Liya; Tilahun, Melaku; Girma, Selfu; Alemayehu, Mekdelawit; Dereje, Abenezer; Assefa, Gebeyehu; Desta, Tigist; Agize, Haymanot; Fisseha, Emnet; Mengistu, Yordanos; Desta, Kassu; Bobosha, Kidist (9 July 2024). "Cytomorphological patterns and clinical features of presumptive tubercular lymphadenitis patients and their comparison with bacteriological detection methods: a cross-sectional study". BMC Infectious Diseases. 24 (1): 684. doi:10.1186/s12879-024-09587-4. ISSN 1471-2334. PMID 38982340.
- ↑ "Clinical Insights into Tuberculous Lymphadenitis" (PDF). Retrieved 2025-09-20.
- ↑ Ganchua, Sharie Keanne C.; White, Alexander G.; Klein, Edwin C.; Flynn, JoAnne L. (August 2020). "Lymph nodes-The neglected battlefield in tuberculosis". PLOS Pathogens. 16 (8): e1008632. doi:10.1371/journal.ppat.1008632. ISSN 1553-7374. PMC 7425845. PMID 32790739.
- ↑ Thakkar, Karan; Ghaisas, Saket Mukund; Singh, Manmohan (2016). "Lymphadenopathy: Differentiation between Tuberculosis and Other Non-Tuberculosis Causes like Follicular Lymphoma". Frontiers in Public Health. 4: 31. Bibcode:2016FrPH....4...31T. doi:10.3389/fpubh.2016.00031. ISSN 2296-2565. PMC 4766275. PMID 26942176.
- ↑ M, Sriram Bhat (30 June 2019). SRB's Manual of Surgery. Jaypee Brothers Medical Publishers. p. 432. ISBN 978-93-5270-907-6.
- ↑ 14.0 14.1 Cockerham, William C. (2016-10-06). International Encyclopedia of Public Health. Academic Press. p. 274. ISBN 9780128037089. Archived from the original on 2023-02-02. Retrieved 2023-01-03.
- ↑ Sharma, Vishal (22 February 2022). Tuberculosis of the Gastrointestinal system. Springer Nature. p. 41. ISBN 978-981-16-9053-2. Retrieved 27 September 2025.
- ↑ 16.0 16.1 Fontanilla, Jose-Mario; Barnes, Arti; von Reyn, C. Fordham (September 2011). "Current diagnosis and management of peripheral tuberculous lymphadenitis". Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 53 (6): 555–562. doi:10.1093/cid/cir454. ISSN 1537-6591. PMID 21865192.
- ↑ 17.0 17.1 Mekonnen, Daniel; Derbie, Awoke; Abeje, Andargachew; Shumet, Abebe; Nibret, Endalkachew; Biadglegne, Fantahun; Munshae, Abaineh; Bobosha, Kidist; Wassie, Liya; Berg, Stefan; Aseffa, Abraham (19 April 2019). "Epidemiology of tuberculous lymphadenitis in Africa: A systematic review and meta-analysis". PLOS ONE. 14 (4): e0215647. Bibcode:2019PLoSO..1415647M. doi:10.1371/journal.pone.0215647. ISSN 1932-6203. PMC 6474617. PMID 31002716.
- ↑ "Tuberculosis (TB)". www.who.int. Archived from the original on 30 July 2020. Retrieved 19 September 2025.
- ↑ "History of World TB Day". World TB Day. 19 February 2025. Archived from the original on 20 September 2025. Retrieved 18 September 2025.
- ↑ Pompermaier, Carolina; Schenato, Mateus Xavier; Franzini, Tales Antunes; Duarte, Fábio Biguelini; Cardoso, Guilherme Roloff (2022). "TUBERCULOUS LYMPHADENITIS: A LITERATURE REVIEW". Mastology. Mastology. p. 81–81. doi:10.29289/259453942022V32S1080.
Further reading
- Yefter, Ermias Teklehaimanot; Taddese, Asefa Adimasu; Tessema, Getahun Mengistu; Limenih, Miteku Andualem; Beyna, Alemante Tafese; Dejen, Addisu Minaye; Alemu, Destaye Shiferaw (17 October 2025). "A clinical scoring system to predict tuberculous lymphadenitis in settings with high disease burden". Scientific Reports. 15 (1): 36439. doi:10.1038/s41598-025-20322-0. ISSN 2045-2322. Retrieved 24 October 2025.
- Chen, Muxing; Zhang, Fan; Yao, Zhixiong; Liu, Yiping; Wu, Di; Chen, Xiaohong; Lin, Youfei (31 December 2025). "Distinctive Immuno-Inflammatory Pattern in Tuberculous Lymphadenitis: A Retrospective Cohort Study with Propensity Score Matching". Infection and Drug Resistance. 18: 4087–4099. doi:10.2147/IDR.S538824.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
External links
| Classification |
|---|