Torus fracture
| Torus fracture | |
|---|---|
| Other names: Buckle fracture | |
 | |
| X-ray of a torus fracture involving the distal radius | |
| Specialty | Emergency medicine |
| Symptoms | Pain[1] |
| Usual onset | 5 and 10 years old[2] |
| Causes | Fall onto an outstretched hand[1] |
| Diagnostic method | Plain X-ray[1] |
| Differential diagnosis | Greenstick fracture, Salter-Harris fracture, toddler’s fracture[3] |
| Treatment | Tensor bandage for up to a few weeks, splint[4][2] |
| Prognosis | Excellent[3] |
| Frequency | Common[1] |
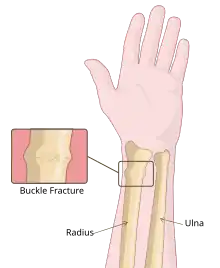
Torus fracture, also known as a buckle fracture, is a type of broken bone that generally occurs in children in which the outer aspect only buckles rather than fully breaks.[2][3] Symptoms generally include pain to the affected area.[1] Associated injuries may include plastic deformation.[3]
It typically results from a fall onto an outstretched hand.[1] Though other causes may include non-accidental injury.[3] The distal forearm is most often affected; though, it may also involve the ribs.[1][2] Diagnosis is generally by X-ray.[1]
A simple soft bandage, like a tensor bandage for up to a few weeks, appears sufficient; with no requirement for dedicated follow-up.[4][1] Pain medications, such as paracetamol and ibuprofen may be used.[1] A removable splint may occasionally be used.[2][3] Torus fractures are common.[1] They generally occur in children between the ages of 5 and 10 years.[2] The name is from the Latin for "protuberance".[2][5]
Signs and symptoms
Torus fractures are low risk and may cause acute pain. As the bone buckles (or crushes), instead of breaking, they are a stable injury as there is no displacement of the bone.[6] This mechanism is analogous to the crumple zones in cars. As with other fractures, the site of fracture may be tender to touch and cause a sharp pain if pressure is exerted on the injured area.
Risk factors
Physical activities or sports such as bike riding or climbing increase the associated risk for buckle fractures in the potential event of a collision or fall. As aforementioned, the most common buckle fracture is of the distal radius in the forearm, which typically originates from a fall onto an outstretched hand (FOOSH).[7] Such orthopaedic injuries are distinctive in children as their bones are softer and in a dynamic state of bone growth and development, with a higher collagen to bone ratio so incomplete fractures such as the buckle fracture are a more common occurrence.[8]
Diagnosis
Buckle fractures can generally be identified by X-ray. The diagnosis is made from both anterior/posterior and lateral projections. The typical features include:
- The buckling of cortical bone, which may appear as a small bulge or protuberance in the radius or ulna.
- The bone may have a slight angulation.[9]
Treatment
.jpg)
The UK's National Institute for Health and Care Excellence (NICE), states that all treatments appeared safe, without the need for a follow-up.[10] A simple soft bandage, like a tensor bandage appears sufficient.[4]
A 2022 study found splint and routine follow-up, or a bandage and no follow-up had equivalent results for pain, function and complications.[11]
Other studies have also shown that parental satisfaction of nearly 100% is achieved when using removable splints that can be taken off at home without the need for outpatient clinics.[12]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Tahir, A; Naji, O; Khawar, H; Iqbal, MJ (30 May 2024). "Torus fractures - diagnosis and management". British journal of hospital medicine (London, England : 2005). 85 (5): 1–8. doi:10.12968/hmed.2023.0336. PMID 38815969.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Worsley, Calum. "Torus fracture". Radiopaedia. Archived from the original on 13 February 2025. Retrieved 27 May 2025.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Asokan, A; Kheir, N (January 2025). "Pediatric Torus Buckle Fracture". StatPearls. PMID 32809469.
- ↑ 4.0 4.1 4.2 Young, Jennifer. "#390 Use the soft touch for buckle fractures? – CFPCLearn". Archived from the original on 25 June 2025. Retrieved 26 May 2025.
- ↑ Wheeless, Clifford R.; Nunley, James A.; Urbaniak, James R. (2016). Wheeless' Textbook of Orthopaedics. Data Trace Internet Publishing, LLC.
- ↑ Randsborg, PH; Sivertsen, EA (October 2009). "Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures". Acta Orthopaedica. 80 (5): 585–9. doi:10.3109/17453670903316850. PMC 2823323. PMID 19916694.
- ↑ van Bosse, HJ; Patel, RJ; Thacker, M; Sala, DA (July 2005). "Minimalistic approach to treating wrist torus fractures". Journal of Pediatric Orthopedics. 25 (4): 495–500. doi:10.1097/01.bpo.0000161098.38716.9b. PMID 15958903. S2CID 33574847.
- ↑ Firmin, F; Crouch, R (July 2009). "Splinting versus casting of "torus" fractures to the distal radius in the paediatric patient presenting at the emergency department (ED): a literature review". International Emergency Nursing. 17 (3): 173–8. doi:10.1016/j.ienj.2009.03.006. PMID 19577205.
- ↑ Patrice Eiff, M.; L. Hatch, Robert (2003). "Boning up on common pediatric fractures". Contemporary Pediatrics. Archived from the original on 2025-06-18. Retrieved 2025-04-28.
- ↑ Nice.org.uk. 2020. Overview | Fractures (Non-Complex): Assessment And Management | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/ng38 Archived 2025-02-24 at the Wayback Machine [Accessed 21 December 2020].
- ↑ Perry, Daniel C.; Achten, Juul; Knight, Ruth; Appelbe, Duncan; Dutton, Susan J.; Dritsaki, Melina; Mason, James M.; Roland, Damian T.; Messahel, Shrouk; Widnall, James; Costa, Matthew L.; Ahmad, Rahail; Alcock, Anastasia; Appelboam, Andrew; Armour, Lisa (2022-07-02). "Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK". The Lancet. 400 (10345): 39–47. doi:10.1016/S0140-6736(22)01015-7. ISSN 0140-6736. PMID 35780790.
- ↑ Solan, MC; Rees, R; Daly, K (July 2002). "Current management of torus fractures of the distal radius". Injury. 33 (6): 503–5. doi:10.1016/s0020-1383(01)00198-x. PMID 12098547.
External links