Hantavirus hemorrhagic fever with renal syndrome
| Hantavirus hemorrhagic fever with renal syndrome | |
|---|---|
| Other names: Hemorrhagic nephrosonephritis[1], Nephropathia epidemica, Korean hemorrhagic fever, epidemic hemorrhagic fever[2] | |
 | |
| Striped field mouse may spread the hantaviruses that cause HFRS[2] | |
| Specialty | Infectious disease |
| Symptoms | Headache, abdominal pain, fever, nausea, blurred vision, rash[2] |
| Complications | Low blood pressure, kidney failure[2] |
| Usual onset | 1 to 2 weeks after exposure[2] |
| Duration | Weeks to months[2] |
| Causes | Certain hantaviruses spread by rodents[2] |
| Diagnostic method | Blood tests[2] |
| Differential diagnosis | Yellow fever, Ebola, sepsis, Dengue, leptospirosis[3] |
| Prevention | Rodent control[2] |
| Treatment | Supportive care[2] |
| Medication | Ribavirin[2] |
| Prognosis | 1 to 15% risk of death[2] |
| Frequency | ~100,000 cases per year[3] |
Hantavirus hemorrhagic fever with renal syndrome (HFRS) is a group of similar illnesses caused by certain hantavirus infections.[2] Initial symptoms generally include headache, abdominal pain, fever, nausea, and blurred vision.[2] Later low blood pressure, kidney failure, and bleeding may occur.[2][3] Onset of initial symptoms is generally 1 to 2 weeks following exposure.[2]
Specifically it is cause by orthohantavirus of the Bunyavirales type.[2] This includes Hantaan orthohantavirus, Dobrava-Belgrade orthohantavirus, Saaremaa virus, Seoul orthohantavirus, and Puumala orthohantavirus.[2] The disease is typically spread when people breath in air contaminated by rodent droppings.[2] Spread between people is very rare.[2] Diagnosis is generally by blood tests.[2] The hantaviruses in the Americas generally result in hantavirus pulmonary syndrome instead.[3]
Prevention is by rodent control.[2] Treatment is primarily supportive care and may include oxygen therapy or dialysis.[2] Ribavirin may be useful if used early.[2] NSAIDs should not be used due to concerns regarding the kidneys.[3] Depending on the virus involved, the risk of death is 1% to 15%.[2] Recovery can take weeks to months; however, people usually recovery fully.[2][3]
About 60,000 to 150,000 cases occur a year.[3] It occurs primarily in Asia and Europe with China and Russia having the most cases.[2][3] In a number of regions males are more commonly affected than females, which is attributed to greater time outdoors.[3] The first clear descriptions of the disease date from the 1930s.[4] The underlying cause was found in 1978.[5]
Signs and symptoms

Symptoms usually develop within 1 to 2 weeks after exposure , but in rare cases, they may take more weeks. In nephropathia epidemica, the incubation period is three weeks. Symptoms begin suddenly and include intense headaches, back and abdominal pain, fever, chills, nausea, and blurred vision. Individuals may have flushing of the face, inflammation or redness of the eyes, or a rash. Later symptoms can include low blood pressure, acute shock, vascular leakage, and acute kidney failure, which can cause severe fluid overload.[3][7][8]
The severity of the disease varies depending upon the virus causing the infection. Hantaan and Dobrava virus infections usually cause severe symptoms, while Seoul, Saaremaa, and Puumala virus infections are usually more moderate. Complete recovery can take weeks or months.[9]
The course of the illness can be split into five phases:
- Fever
- Symptoms include redness of cheeks and nose, fever, chills, sweaty palms, diarrhea, malaise, headaches, nausea, abdominal and back pain, respiratory problems such as the ones common in the influenza virus, as well as gastro-intestinal problems. These symptoms normally occur for three to seven days and arise about two to three weeks after exposure.[10]
- Low blood pressure
- This occurs when the blood platelet levels drop and symptoms can lead to tachycardia and hypoxemia. This phase can last for a few days.[11]
- Low urine output
- This phase lasts for three to seven days and is characterised by the onset of renal failure and proteinuria.[11]
- High urine output
- This is characterized by diuresis of several litres per day, which can last for a couple of days up to weeks.[12][13]
- Recovery
- This is normally when recovery occurs and symptoms begin to improve.[12]
This syndrome can also be fatal. In some cases, it has been known to cause permanent renal failure.[14]
Cause
.jpg)
The cause is one of four hantaviruses:[3][15]
- Hantaan virus is most common cause of HFRS and causes a severe form of disease. [16]
- Seoul virus is found worldwide, causes a moderate form of HFRS[17]
- Puumala virus is in Russia and northern and central Europe,usually causes a mild form [18]
- Dobrava-Belgrade virus is in southern Europe,severity depending on its genotype.[19]
Transmission
Transmission by aerosolized rodent excreta still remains the only known way the virus is transmitted to humans. In general, droplet and/or fomite transfer has not been shown in the hantaviruses in either the pulmonary or hemorrhagic forms.[20][21]
For Nephropathia epidemica, the bank vole is the reservoir for the virus, which humans contract through inhalation of aerosolised vole droppings.[22]
Mechanism
The pathogenesis of this condition indicates that 3 weeks is the incubation period for the virus. The virus causes vascular endothelial damage which causes loss of plasma, hypotension.[3]
The virus enters the body through inhalation of aerosolized particles. It targets vascular endothelial cells and macrophages, which leads to widespread infection. Hantaviruses cause increased vascular permeability by infecting endothelial cells. This results in fluid leakage, which is responsible for many of the severe symptoms, including shock. The immune system's response to the virus can exacerbate the damage. Cytokine release and immune cell activation contribute to inflammation and more vascular damage. The kidneys are affected, leading to acute kidney injury.[3][23]
In short apparently the virus enters via beta-3 integrins receptors and then forces cytoskeletal reorganization. Additionally a severe immunological reaction of this condition can be a cytokine storm.[3]
-
![Mechanism of Hantavirus induced AKI[13]](./_assets_/0c70a452f799bfe840676ee341124611/Hantavirus_hemorrhagic_fever_with_renal_syndrome.jpg) Mechanism of Hantavirus induced AKI[13]
Mechanism of Hantavirus induced AKI[13] -
![Orthohantavirus infection portal of entry and initial replication sites[24][3]](./_assets_/0c70a452f799bfe840676ee341124611/Hantavirus_hemorrhagic_fever_with_renal_syndrome.webp.png)
Diagnosis
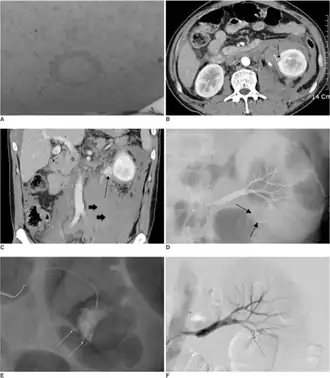
HFRS is difficult to diagnose on clinical grounds alone and serological evidence is often needed. A fourfold rise in IgG antibody titer in a 1-week interval and the presence of the IgM type of antibodies against hantaviruses are good evidence for an acute hantavirus infection. HFRS should be suspected in patients with acute febrile flu-like illness, kidney failure of unknown origin and sometimes liver dysfunction.[25]
Differential diagnosis
The DDx in an individual with HFRS is as follows:[3]
- Septicemia
- Ebola
- Dengue
- Leptospirosis
- Yellow fever
- Malaria
- Murine typhus
- Disseminated intravascular coagulation
- Thrombotic thrombocytopenic purpura
Prevention
Rodent control in and around the home remains the primary prevention strategy, as well as eliminating contact with rodents in the workplace and campsite. Closed storage sheds and cabins are often ideal sites for rodent infestations. Airing out of such spaces prior to use is recommended. Avoid direct contact with rodent droppings and wear a mask to avoid inhalation of aerosolized rodent secretions.[26]
Treatment
There is no cure for HFRS. Treatment involves supportive therapy including renal dialysis. Treatment with ribavirin , administered within 7 days of onset of fever, resulted in a reduced mortality as well as shortened course of illness.[9][10][15]
Epidemiology
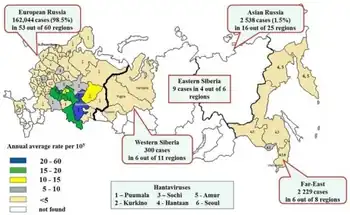
HFRS is primarily a Eurasian disease, whereas HPS appears to be confined to the Americas. [25]
The geography is directly related to the indigenous rodent hosts and the viruses that coevolved with them.[25]
Although fatal in a small percentage of cases, nephropathia epidemica is generally milder than the HFRS that is caused by hantaviruses in other parts of the world.[28]
History

Hantavirus hemorrhagic fever with renal syndrome was first identified and studied during the Korean War in the early 1950s. [29][30]
The disease was linked to the Hantaan virus, which was discovered by Dr. Ho Wang Lee, in 1976. His work helped establish the connection between the virus and the disease[29]
This infection is known as sorkfeber in Swedish and myyräkuume in Finnish (vole fever). In Norway, it is called musepest (mouse plague).[31]
References
- ↑ "Hantavirus hemorrhagic fever with renal syndrome (Concept Id: CN281780) - MedGen - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2 March 2025.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 "CDC - Hemorrhagic Fever with Renal Syndrome (HFRS) - Hantavirus". www.cdc.gov. 22 February 2019. Archived from the original on 16 November 2019. Retrieved 29 March 2021.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 Romero, MG; Anjum, F (January 2021). "Hemorrhagic Fever Renal Syndrome". StatPearls. PMID 32809495.
- ↑ Emerging Infectious Diseases. National Center for Infectious Diseases, Centers for Disease Control and Prevention (CDC). 2010. p. 1195. Archived from the original on 2021-08-28. Retrieved 2021-03-29.
- ↑ Schmaljohn, C.; Nichol, S. T. (2000). Hantaviruses. Springer Science & Business Media. p. 92. ISBN 978-3-642-56753-7. Archived from the original on 2021-08-28. Retrieved 2021-03-29.
- ↑ Avellaneda-Campos, R. (January 2012). "Fiebre hemorrágica con síndrome renal: a propósito de un caso". Nefrología. 32 (32): 131–132. doi:10.3265/Nefrologia.pre2011.Dec.11225. PMID 22294021.
- ↑ Tariq, Misbah; Kim, Dong-Min (2022). "Hemorrhagic Fever with Renal Syndrome: Literature Review, Epidemiology, Clinical Picture and Pathogenesis". Infection & Chemotherapy. 54 (1): 1–19. doi:10.3947/ic.2021.0148. PMC 8987181. PMID 35384417.
- ↑ Maftei, Irinel-Doina; Segall, Liviu; Panculescu-Gatej, Raluca; Ceianu, Cornelia; Covic, Adrian (1 August 2012). "Hantavirus infection—Hemorrhagic fever with renal syndrome: the first case series reported in Romania and review of the literature". International Urology and Nephrology. 44 (4): 1185–1191. doi:10.1007/s11255-011-0013-z. ISSN 1573-2584. PMID 21678038. Retrieved 11 March 2025.
- ↑ 9.0 9.1 Lee HW, van der Groen G (1989). "Hemorrhagic fever with renal syndrome". Prog. Med. Virol. 36: 62–102. PMID 2573914.
- ↑ 10.0 10.1 Muranyi, Walter; Bahr, Udo; Zeier, Martin; Van Der Woude, Fokko J. (2005). "Hantavirus Infection". Journal of the American Society of Nephrology. 16 (12): 3669–3679. doi:10.1681/ASN.2005050561. PMID 16267154. Archived from the original on 2018-09-04. Retrieved 2020-03-25.
- ↑ 11.0 11.1 Canada, Public Health Agency of (19 August 2011). "Pathogen Safety Data Sheets: Infectious Substances – Hantavirus spp". www.canada.ca. Retrieved 10 March 2025.
- ↑ 12.0 12.1 Fulhorst, Charles F.; Koster, Frederick T.; Enría, Delia A.; Peters, C. J. (1 January 2011). "CHAPTER 71 - Hantavirus Infections". Tropical Infectious Diseases: Principles, Pathogens and Practice (Third ed.). W.B. Saunders. pp. 470–480. ISBN 978-0-7020-3935-5.
- ↑ 13.0 13.1 Mir, Sheema (18 January 2022). "Hantavirus Induced Kidney Disease". Frontiers in Medicine. 8. doi:10.3389/fmed.2021.795340. PMC 8804099. PMID 35118091.
- ↑ Kulzer P, Heidland A (December 1994). "[Acute kidney failure caused by Hantaviruses]". Ther Umsch (in Deutsch). 51 (12): 824–31. PMID 7784996.
- ↑ 15.0 15.1 "Clinician Brief: Hemorrhagic Fever with Renal Syndrome". Hantavirus. 23 May 2024. Retrieved 5 April 2025.
- ↑ Yu, Xue-jie; Tesh, Robert B. (1 December 2014). "The Role of Mites in the Transmission and Maintenance of Hantaan Virus (Hantavirus: Bunyaviridae)". The Journal of Infectious Diseases. 210 (11): 1693–1699. doi:10.1093/infdis/jiu336. ISSN 0022-1899. PMC 4296190. PMID 24958909.
- ↑ "Seoul virus – United States of America and Canada". www.who.int. Retrieved 5 March 2025.
- ↑ Meyer, Barbara J; Schmaljohn, Connie S (1 February 2000). "Persistent hantavirus infections: characteristics and mechanisms". Trends in Microbiology. 8 (2): 61–67. doi:10.1016/S0966-842X(99)01658-3. ISSN 0966-842X. PMID 10664598.
- ↑ Papa, Anna (August 2012). "Dobrava-Belgrade virus: phylogeny, epidemiology, disease". Antiviral Research. 95 (2): 104–117. doi:10.1016/j.antiviral.2012.05.011. ISSN 1872-9096. PMID 22659378.
- ↑ Peters CJ (2006). "Emerging infections: lessons from the viral hemorrhagic fevers". Trans. Am. Clin. Climatol. Assoc. 117: 189–96, discussion 196–7. PMC 1500910. PMID 18528473.
- ↑ Crowley, J.; Crusberg, T. "Ebola and Marburg Virus Genomic Structure, Comparative and Molecular Biology". Dept. of Biology & Biotechnology, Worcester Polytechnic Institute. Archived from the original on 2013-10-15.
- ↑ Rose AM, Vapalahti O, Lyytikäinen O, Nuorti P (January 2003). "Patterns of Puumala virus infection in Finland". Euro Surveill. 8 (1): 9–13. doi:10.2807/esm.08.01.00394-en. PMID 12631978.
- ↑ Lupuşoru, Gabriela; Lupuşoru, Mircea; Ailincăi, Ioana; Bernea, Lavinia; Berechet, Andreea; Spătaru, Radu; Ismail, Gener (12 July 2021). "Hanta hemorrhagic fever with renal syndrome: A pathology in whose diagnosis kidney biopsy plays a major role (Review)". Experimental and Therapeutic Medicine. 22 (3): 984. doi:10.3892/etm.2021.10416. PMC 8311249. PMID 34345266.
Hantaviruses infect the susceptible cells by interaction of the viral envelope glycoproteins with β-integrin surface molecules.
- ↑ Sehgal, Ayushi; Mehta, Sanya; Sahay, Kritika; Martynova, Ekaterina; Rizvanov, Albert; Baranwal, Manoj; Chandy, Sara; Khaiboullina, Svetlana; Kabwe, Emmanuel; Davidyuk, Yuriy (18 February 2023). "Hemorrhagic Fever with Renal Syndrome in Asia: History, Pathogenesis, Diagnosis, Treatment, and Prevention". Viruses. 15 (2): 561. doi:10.3390/v15020561. ISSN 1999-4915. PMC 9966805. PMID 36851775.
- ↑ 25.0 25.1 25.2 Peters CJ, Simpson GL, Levy H (1999). "Spectrum of hantavirus infection: hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome". Annu. Rev. Med. 50: 531–45. doi:10.1146/annurev.med.50.1.531. PMID 10073292.
- ↑ "CDC - Hantavirus Pulmonary Syndrome (HPS) - Hantavirus". Cdc.gov. 2013-02-06. Archived from the original on 2013-05-24. Retrieved 2013-07-07.
- ↑ Tkachenko, Evgeniy; Kurashova, Svetlana; Balkina, Alexandra; Ivanov, Alexander; Egorova, Mariya; Leonovich, Oksana; Popova, Yulia; Teodorovich, Rostislav; Belyakova, Alla; Tkachenko, Petr; Trankvilevsky, Dmitriy; Blinova, Ekaterina; Ishmukhametov, Aydar; Dzagurova, Tamara (12 July 2023). "Cases of Hemorrhagic Fever with Renal Syndrome in Russia during 2000-2022". Viruses. 15 (7): 1537. doi:10.3390/v15071537. ISSN 1999-4915. PMC 10383633. PMID 37515224.
- ↑ Jonsson CB, Figueiredo LT, Vapalahti O (April 2010). "A global perspective on hantavirus ecology, epidemiology, and disease". Clin. Microbiol. Rev. 23 (2): 412–41. doi:10.1128/CMR.00062-09. PMC 2863364. PMID 20375360.
- ↑ 29.0 29.1 Song, Jin-Won (2022). "In Memoriam: Professor Ho Wang Lee (1928–2022)". Journal of Korean Medical Science. 37 (36): e274. doi:10.3346/jkms.2022.37.e274. PMC 9485066.
- ↑ Cameron, J. Stewart (1 June 2001). "The history of viral haemorrhagic fever with renal disease (hantavirus)". Nephrology Dialysis Transplantation. 16 (6): 1289–1290. doi:10.1093/ndt/16.6.1289. ISSN 0931-0509.
- ↑ "Hantavirus Hemorrhagic Fever with Renal Syndrome disease: Malacards - Research Articles, Drugs, Genes, Clinical Trials". www.malacards.org. Retrieved 11 March 2025.
External links
| Classification |
|---|