Neuroborreliosis
| Neuroborreliosis | |
|---|---|
| Other names: Lyme neuroborreliosis (LNB)[1] | |
  | |
| |
| Specialty | Infectious disease,neurology |
| Symptoms | Facial nerve palsy, and radiculoneuritis [2] |
| Causes | Complication of Lyme disease[3][4] |
| Diagnostic method | Antibody test[5][6] |
| Differential diagnosis | Acute disseminated encephalomyelitis, viral meningitis, Multiple sclerosis, Bell's palsy[7][8] |
| Treatment | Ceftriaxone or penicillin G[9] |
Neuroborreliosis is a disorder of the central nervous system. A neurological manifestation of Lyme disease, neuroborreliosis is caused by a systemic infection of spirochetes of the genus Borrelia.[10] Symptoms of the disease include erythema migrans and flu-like symptoms.[11]
Neuroborreliosis is treated with intravenous antibiotics such as penicillins, or cefotaxime.[9]
In terms of the epidemiology of Lyme neuroborreliosis we find it varies by region[2].
Signs and symptoms
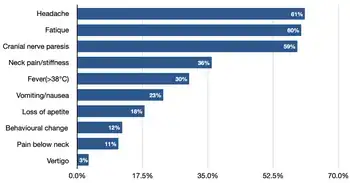
Neuroborreliosis is often preceded by the typical symptoms of Lyme disease, which include erythema migrans and flu-like symptoms such as fever and muscle aches. Neurologic symptoms of neuroborreliosis include the meningoradiculitis, cranial nerve abnormalities, and altered mental status. Sensory findings may also be present. Rarely, a progressive form of encephalomyelitis may occur. In children, symptoms of neuroborreliosis include headache, sleep disturbance, and symptoms associated with increased intracranial pressure, such as papilledema. Less common childhood symptoms can include meningitis, myelitis, ataxia, and chorea. Ocular Lyme disease has also been reported, as has neuroborreliosis affecting the spinal cord, but neither of these findings are common.[2]
Cause
As to the etiology we find that Borrelia burgdorferi sensu stricto is the primary cause of Lyme disease and subsequent neuroborreliosis in North America, in Europe, neuroborreliosis can be caused by Borrelia burgdorferi sensu stricto, but more commonly by other Borrelia species within the Borrelia burgdorferi sensu lato complex, particularly Borrelia garinii and Borrelia afzelii.[3][4]
Mechanism
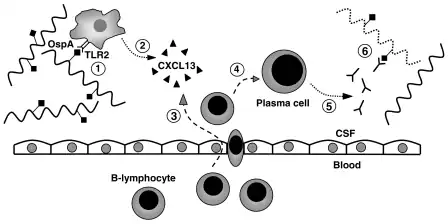
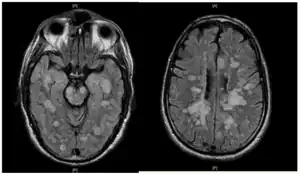
In terms of the mechanism we find that once infection has occurred the bacteria evades the host's immune system to survive and spread. Borrelia burgdorferi penetrates the blood-brain barrier, allowing it to enter the cerebrospinal fluid.Once in the CSF, the bacteria trigger an immune response, leading to inflammation.[12][10]
Immune evasion by B. burgdorferi occurs via changing the expression of surface proteins like VlsE which helps the bacteria evade antibody recognition.Reducing the expression of immunogenic surface proteins can limit immune recognition.Expressing complement regulatory-acquiring surface proteins allows the spirochetes to resist complement-mediated killing. [13][14][1][15][2]And finally, B. burgdorferi can induce the production of anti-inflammatory cytokines, diminishing the host's immune response.IL-10 can dampen the inflammatory response by inhibiting the release and function of pro-inflammatory cytokines like TNF-alpha, IFN-gamma[16]
Diagnosis
Diagnosis is determined by clinical examination of visible symptoms.[5] Neuroborreliosis can also be diagnosed serologically to confirm clinical examination via western blot, ELISA, and PCR.[6]
Differential diagnosis
A number of diseases can produce symptoms similar to those of Lyme neuroborreliosis. They include: [8][7]
Treatment
In the US, neuroborreliosis is typically treated with intravenous antibiotics which cross the blood–brain barrier, such as penicillins, ceftriaxone, or cefotaxime.[9]
Small observational studies suggest ceftriaxone is also effective in children.[17] The recommended duration of treatment is 14 to 28 days.[18][19]Several studies from Europe have suggested oral doxycycline is equally as effective as intravenous ceftriaxone in treating neuroborreliosis. Doxycycline has not been widely studied as a treatment in the US, but antibiotic sensitivities of prevailing European and US isolates of Borrelia burgdorferi tend to be identical. However, doxycycline is generally not prescribed to children due to the risk of bone and tooth damage.[9]
Prognosis
The prognosis for Lyme neuroborreliosis is good with appropriate antibiotic treatment. However, some individuals may experience symptoms even after eradication of infection; some studies indicated that 28 percent of patients might have residual neurological or cognitive symptoms after LNB.[20]
Epidemiology
As to the epidemiology of Lyme neuroborreliosis varies by region. In United States, it is primarily caused by Borrelia burgdorferi sensu stricto, whereas in Europe, Borrelia garinii and Borrelia afzelii are more common. The incidence of Lyme disease is influenced by geography and seasonality[2].
History

Lyme Neuroborreliosis is a neurological manifestation of Lyme disease, which is caused by the bacterium Borrelia burgdorferi;the discovery of Lyme disease itself is credited to Dr. Willy Burgdorfer, who identified the connection between the deer tick and the disease in 1981. His research led to the naming of the bacterium Borrelia burgdorferi in his honor.[21]
Research
Research is ongoing to identify new biomarkers in both CSF and blood to improve the diagnosis of Neuroborreliosis . While CXCL13 in CSF is commonly used, the diagnosis of LNB faces challenges, in early stages or in atypical presentations. NfL is a protein component of neuronal axons, and its elevated levels in CSF and blood indicate neuronal damage or degeneration. It's a general marker of neuro-axonal injury, not specific to LNB, but its role in assessing disease severity and prognosis in LNB is being explored.[22]
See also
Notes
- 1.^ Articles are Pubmed indexed but not reviews
References
- ↑ 1.0 1.1 Kozak, Sylwia; Kaminiów, Konrad; Kozak, Katarzyna; Paprocka, Justyna (7 June 2021). "Lyme Neuroborreliosis in Children". Brain Sciences. 11 (6): 758. doi:10.3390/brainsci11060758. ISSN 2076-3425. PMC 8226969. PMID 34200467.
- ↑ 2.0 2.1 2.2 2.3 Hildenbrand, P.; Craven, D. E.; Jones, R.; Nemeskal, P. (1 June 2009). "Lyme Neuroborreliosis: Manifestations of a Rapidly Emerging Zoonosis". American Journal of Neuroradiology. 30 (6): 1079–1087. doi:10.3174/ajnr.A1579. ISSN 0195-6108. PMC 7051319. PMID 19346313. Archived from the original on 8 February 2025. Retrieved 8 May 2025. Archived 8 February 2025 at the Wayback Machine
- ↑ 3.0 3.1 Ogrinc, Katarina; Maraspin, Vera (28 March 2016). "Nervous System Involvement in Lyme Borreliosis" (PDF). The Open Dermatology Journal. 10 (1): 44–54. doi:10.2174/1874372201610010044.
- ↑ 4.0 4.1 Shapiro, Eugene D. (1 December 2014). "Borrelia burgdorferi (Lyme Disease)". Pediatrics in Review. 35 (12): 500–509. doi:10.1542/pir.35-12-500. ISSN 0191-9601. PMC 5029759. PMID 25452659.
- ↑ 5.0 5.1 Meyerhoff JO, Zaidman GW and Steele RW for Medscape Drugs & Diseases, Eds. Diamond HS et al. Lyme Disease Differential Diagnoses: Diagnostic Considerations Archived 2023-05-06 at the Wayback Machine Updated: Mar 14, 2016
- ↑ 6.0 6.1 CDC Two-step Laboratory Testing Process Archived 2015-03-12 at the Wayback Machine Page last reviewed: March 4, 2015. Page last updated: March 26, 2015
- ↑ 7.0 7.1 Mygland, A.; Ljøstad, U.; Fingerle, V.; Rupprecht, T.; Schmutzhard, E.; Steiner, I. (January 2010). "EFNS guidelines on the diagnosis and management of European Lyme neuroborreliosis". European Journal of Neurology. 17 (1): 8–16, e1–4. doi:10.1111/j.1468-1331.2009.02862.x. ISSN 1468-1331. PMID 19930447. Archived from the original on 2025-02-04. Retrieved 2025-05-10.
- ↑ 8.0 8.1 Lyme Disease at eMedicine
- ↑ 9.0 9.1 9.2 9.3 Halperin, John J. (June 2008). "Nervous System Lyme Disease". Infectious Disease Clinics of North America. 22 (2): 261–74, vi. doi:10.1016/j.idc.2007.12.009. PMID 18452800. S2CID 10590435.
- ↑ 10.0 10.1 10.2 Rupprecht, Tobias A.; Koedel, Uwe; Fingerle, Volker; Pfister, Hans-Walter (March 2008). "The Pathogenesis of Lyme Neuroborreliosis: From Infection to Inflammation". Molecular Medicine. 14 (3): 205–212. doi:10.2119/2007-00091.Rupprecht. ISSN 1528-3658.
- ↑ Koedel, Uwe; Fingerle, Volker; Pfister, Hans-Walter (2015-08-01). "Lyme neuroborreliosis-epidemiology, diagnosis and management". Nature Reviews. Neurology. 11 (8): 446–456. doi:10.1038/nrneurol.2015.121. ISSN 1759-4766. PMID 26215621. S2CID 13694627.
- ↑ Ford, Lenzie; Tufts, Danielle M. (15 June 2021). "Lyme Neuroborreliosis: Mechanisms of B. burgdorferi Infection of the Nervous System". Brain Sciences. 11 (6): 789. doi:10.3390/brainsci11060789. ISSN 2076-3425. PMC 8232152. PMID 34203671.
- ↑ Anderson, Cassidy; Brissette, Catherine A. (2 March 2021). "The Brilliance of Borrelia: Mechanisms of Host Immune Evasion by Lyme Disease-Causing Spirochetes". Pathogens (Basel, Switzerland). 10 (3): 281. doi:10.3390/pathogens10030281. ISSN 2076-0817. PMC 8001052. PMID 33801255.
- ↑ Brooks, Chad S.; Vuppala, Santosh R.; Jett, Amy M.; Akins, Darrin R. (January 2006). "Identification of Borrelia burgdorferi outer surface proteins". Infection and Immunity. 74 (1): 296–304. doi:10.1128/IAI.74.1.296-304.2006. ISSN 0019-9567. PMC 1346608. PMID 16368984.
- ↑ Rogovskyy, Artem S.; Bankhead, Troy (2013). "Variable VlsE is critical for host reinfection by the Lyme disease spirochete". PLOS ONE. 8 (4): e61226. Bibcode:2013PLoSO...861226R. doi:10.1371/journal.pone.0061226. ISSN 1932-6203. PMC 3620393. PMID 23593438.
- ↑ Saraiva, Margarida; Vieira, Paulo; O'Garra, Anne (14 October 2019). "Biology and therapeutic potential of interleukin-10". Journal of Experimental Medicine. 217 (1): e20190418. doi:10.1084/jem.20190418. ISSN 0022-1007. PMC 7037253. PMID 31611251. Archived from the original on 28 March 2025. Retrieved 12 May 2025. Archived 28 March 2025 at the Wayback Machine
- ↑ Bloom, Bradley J.; Wyckoff, Patricia M.; Meissner, H. Cody; Steere, Allen C. (March 1998). "Neurocognitive abnormalities in children after classic manifestations of Lyme disease". The Pediatric Infectious Disease Journal. 17 (3): 189–96. doi:10.1097/00006454-199803000-00004. PMID 9535244.
- ↑ Wormser, G. P.; Dattwyler, R. J.; Shapiro, E. D.; Halperin, J. J.; Steere, A. C.; Klempner, M. S.; Krause, P. J.; Bakken, J. S.; Strle, F.; Stanek, G.; Bockenstedt, L.; Fish, D.; Dumler, J. S.; Nadelman, R. B. (November 2006). "The Clinical Assessment, Treatment, and Prevention of Lyme Disease, Human Granulocytic Anaplasmosis, and Babesiosis: Clinical Practice Guidelines by the Infectious Diseases Society of America". Clinical Infectious Diseases. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130.
- ↑ Halperin, J. J.; Shapiro, E. D.; Logigian, E.; Belman, A. L.; Dotevall, L.; Wormser, G. P.; Krupp, L.; Gronseth, G.; Bever, C. T. (July 2007). "Practice Parameter: Treatment of nervous system Lyme disease (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 69 (1): 91–102. doi:10.1212/01.wnl.0000265517.66976.28. PMID 17522387.
- ↑ Dersch, R.; Sommer, H.; Rauer, S.; Meerpohl, J. J. (1 January 2016). "Prevalence and spectrum of residual symptoms in Lyme neuroborreliosis after pharmacological treatment: a systematic review". Journal of Neurology. 263 (1): 17–24. doi:10.1007/s00415-015-7923-0. ISSN 1432-1459. PMID 26459093. Archived from the original on 30 September 2022. Retrieved 13 May 2025. Archived 30 September 2022 at the Wayback Machine
- ↑ "The Myths of Lyme Disease: Separating Fact from Fiction for Military Personnel". NDU press. Retrieved 7 May 2025.
- ↑ Skarstein, Ingerid; Ulvestad, Elling; Solheim, Anne Marit; Vedeler, Christian; Ljøstad, Unn; Mygland, Åse; Eikeland, Randi; Reiso, Harald; Lorentzen, Åslaug Rudjord; Bos, Steffan Daniel (May 2024). "Serum neurofilament light chain associates with symptom burden in Lyme neuroborreliosis patients: a longitudinal cohort study from Norway". Journal of Neurology. 271 (5): 2768–2775. doi:10.1007/s00415-024-12237-z. ISSN 1432-1459. Archived from the original on 2025-02-04. Retrieved 2025-07-21.
Further reading
- Bruinsma, R. A.; Skogman, B. H.; van Hensbroek, M. Boele; Vermeeren, Y. M.; Hovius, J. W.; Zomer, T. P. (2 July 2025). "Long-term clinical outcomes after Lyme neuroborreliosis in children". BMC pediatrics. 25 (1): 511. doi:10.1186/s12887-025-05782-7. ISSN 1471-2431.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
External links
| Classification |
|
|---|