Asystole
| Asystole | |
|---|---|
| Other names: Cardiac flatline, asystolic arrest | |
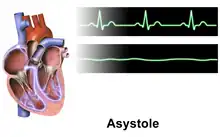
| A rhythm strip showing two beats of normal sinus rhythm followed by an atrial beat and asystole | |
| Pronunciation |
|
| Symptoms | Unresponsive, no pulse[1] |
| Complications | Brain damage[2] |
| Causes | Hs and Ts: hypoxia, hyperkalemia, hypovolemia, hypothermia, cardiac thrombosis, pulmonary thrombosis, tamponade, tension pneumothorax, toxins[3] |
| Diagnostic method | ECG showing a more or less flat line[3][4] |
| Differential diagnosis | Fine ventricular fibrillation, PEA[1][2] |
| Treatment | CPR, epinephrine[5] |
| Prognosis | Very poor[3] |
| Deaths | >98% risk of death[3] |
Asystole is when there is neither movement nor electrical activity from the ventricle of the heart.[2] The person is unresponsive, not breathing properly, and without a pulse.[1][6] Gasping breaths may be present.[2] It is the type of cardiac arrest with the worst outcomes, and is usually irreversible.[3] Among those who survive, brain damage may have occurred.[2]
Causes include the Hs and Ts: hypoxia, hyperkalemia, hypovolemia, hypothermia, cardiac thrombosis, pulmonary thrombosis, tamponade, tension pneumothorax, and toxins.[3] It often occurs after a period of pulseless electrical activity or ventricular fibrillation.[6] The underlying mechanism results in no cardiac output.[3] Diagnosis is by an ECG showing a more or less flat line which may wonder a bit.[3][4] In a different context, some have defined it as a sinus pause greater than 3 seconds, but this may be better termed sinus arrest.[7][8] The monitor connections should be checked and the rhythm verified in multiple leads.[2][4]
Treatment is with cardiopulmonary resuscitation (CPR) and epinephrine.[5] Epinephrine is generally given as early as possible at a dose of 1 mg intravenously every 3–5 minutes.[9][2] Shocking the person, pacing, and atropine are not generally useful.[3][10][6] Evidence dose not support the use of a precordial thump.[6] Prolonged resuscitation efforts are rarely indicated.[1]
Asystole is found initially in about half of out-of-hospital cardiac arrests and 28% of among hospitalized people.[11][1][12] Survival in out-of-hospital cases is less than 2% and in-hospital cases is about 10%.[3] Good neurological outcomes occurred in less than 1% of people.[11] It is New Latin, from Greek privative a meaning "not, without" and systolē meaning "contraction".[13][14]
Cause
Possible underlying causes, which may be treatable and reversible in certain cases, include the Hs and Ts.[15][16][17]
- Hypovolemia
- Hypoxia
- Hydrogen ions (acidosis)
- Hypothermia
- Hyperkalemia or hypokalemia
- Toxins (e.g. drug overdose)
- Cardiac tamponade
- Tension pneumothorax
- Thrombosis (myocardial infarction or pulmonary embolism)
While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage (when the chest is opened and the heart is manually compressed) is performed, and even then it is a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm reappears, if asystole has persisted for fifteen minutes or more, the brain will have been deprived of oxygen long enough to cause severe hypoxic brain damage, resulting in brain death or persistent vegetative state.[18]
-
ECG lead showing asystole (flatline)
-
 Asystole
Asystole -
 Ventricular fibrillation
Ventricular fibrillation
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Jordan, MR; Lopez, RA; Morrisonponce, D; Flynn, L (January 2025). "Asystole (Nursing)". StatPearls. PMID 33760533.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Jordan, MR; Lopez, RA; Morrisonponce, D (January 2025). "Asystole". StatPearls. PMID 28613616.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 Bell, Daniel; Vadera, Sonam (7 April 2020). "Asystole". Radiopaedia.org. Radiopaedia.org. doi:10.53347/rID-75785. Archived from the original on 5 June 2024. Retrieved 25 February 2025.
- ↑ 4.0 4.1 4.2 Aitken, Leanne; Marshall, Andrea; Buckley, Thomas (19 December 2023). Critical Care Nursing. Elsevier Health Sciences. p. 349. ISBN 978-0-7295-9827-9. Archived from the original on 12 April 2025. Retrieved 27 February 2025.
- ↑ 5.0 5.1 Kempton, Hannah; Vlok, Ruan; Thang, Christopher; Melhuish, Thomas; White, Leigh (March 2019). "Standard dose epinephrine versus placebo in out of hospital cardiac arrest: A systematic review and meta-analysis". The American Journal of Emergency Medicine. 37 (3): 511–517. doi:10.1016/j.ajem.2018.12.055. PMID 30658877. S2CID 58580872.
- ↑ 6.0 6.1 6.2 6.3 Neumar, R. W.; Otto, C. W.; Link, M. S.; Kronick, S. L.; Shuster, M.; Callaway, C. W.; Kudenchuk, P. J.; Ornato, J. P.; McNally, B.; Silvers, S. M.; Passman, R. S.; White, R. D.; Hess, E. P.; Tang, W.; Davis, D.; Sinz, E.; Morrison, L. J. (17 October 2010). "Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18_suppl_3): S729 – S767. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224.
- ↑ Berry, Richard B. (18 July 2011). Fundamentals of Sleep Medicine E-Book: Expert Consult - Online and Print. Elsevier Health Sciences. p. 165. ISBN 978-1-4557-1123-9. Archived from the original on 12 April 2025. Retrieved 27 February 2025.
- ↑ Burns, Ed; Buttner, Robert; Buttner, Ed Burns and Robert (1 August 2018). "Sinus Node Dysfunction (Sick Sinus Syndrome)". Life in the Fast Lane • LITFL. Archived from the original on 15 January 2025. Retrieved 27 February 2025.
- ↑ Berg, KM; Soar, J; Andersen, LW; Böttiger, BW; Cacciola, S; Callaway, CW; Couper, K; Cronberg, T; D'Arrigo, S; Deakin, CD; Donnino, MW; Drennan, IR; Granfeldt, A; Hoedemaekers, CWE; Holmberg, MJ; Hsu, CH; Kamps, M; Musiol, S; Nation, KJ; Neumar, RW; Nicholson, T; O'Neil, BJ; Otto, Q; de Paiva, EF; Parr, MJA; Reynolds, JC; Sandroni, C; Scholefield, BR; Skrifvars, MB; Wang, TL; Wetsch, WA; Yeung, J; Morley, PT; Morrison, LJ; Welsford, M; Hazinski, MF; Nolan, JP; Adult Advanced Life Support, Collaborators (20 October 2020). "Adult Advanced Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations". Circulation. 142 (16_suppl_1): S92 – S139. doi:10.1161/CIR.0000000000000893. PMID 33084390.
{{cite journal}}:|first38=has generic name (help) - ↑ Panchal, AR; Bartos, JA; Cabañas, JG; Donnino, MW; Drennan, IR; Hirsch, KG; Kudenchuk, PJ; Kurz, MC; Lavonas, EJ; Morley, PT; O'Neil, BJ; Peberdy, MA; Rittenberger, JC; Rodriguez, AJ; Sawyer, KN; Berg, KM; Adult Basic and Advanced Life Support Writing, Group (20 October 2020). "Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 142 (16_suppl_2): S366 – S468. doi:10.1161/CIR.0000000000000916. PMID 33081529.
{{cite journal}}:|first17=has generic name (help) - ↑ 11.0 11.1 Dwivedi, DB; Ball, J; Smith, K; Nehme, Z (July 2025). "Incidence and outcomes of out-of-hospital cardiac arrest from initial asystole: a systematic review and meta-analysis". Resuscitation. 212: 110629. doi:10.1016/j.resuscitation.2025.110629. PMID 40324517.
- ↑ Baldzizhar, Aksana; Manuylova, Ekaterina; Marchenko, Roman; Kryvalap, Yury; Carey, Mary G. (September 2016). "Ventricular Tachycardias". Critical Care Nursing Clinics of North America. 28 (3): 317–329. doi:10.1016/j.cnc.2016.04.004. PMID 27484660.
- ↑ "asystole | Etymology of asystole by etymonline". www.etymonline.com. Archived from the original on 26 January 2021. Retrieved 27 February 2025.
- ↑ "Henry George Liddell, Robert Scott, A Greek-English Lexicon, συστολ-ή". www.perseus.tufts.edu. Archived from the original on 7 May 2021. Retrieved 27 February 2025.
- ↑ Mazur G (2004). ACLS: Principles And Practice. Dallas: American Heart Association. pp. 71–87. ISBN 978-0-87493-341-3.
- ↑ Barnes TG, Cummins RO, Field J, Hazinski MF (2003). ACLS for experienced providers. Dallas: American Heart Association. pp. 3–5. ISBN 978-0-87493-424-3.
- ↑ ECC Committee, Subcommittees and Task Forces of the American Heart Association (December 2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care – Part 7.2: Management of Cardiac Arrest". Circulation. 112 (24 Suppl): IV1–203 (7.2 IV58–66). doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375.
- ↑ Shah, Sandy (16 October 2021). "Asystole: Background, Pathophysiology, Etiology". eMedicine. Archived from the original on 4 December 2008. Retrieved 30 March 2024.
External links
| Classification |
|---|