Golfer's elbow
| Golfer's elbow | |
|---|---|
| Other names: Medial epicondylitis; pitcher's elbow; medial epicondylalgia; medial tendinosis;[1] medial tennis elbow[2] | |
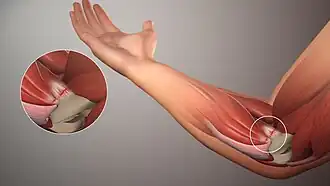
| Left elbow-joint, showing anterior and ulnar collateral ligaments. Medial epicondyle labeled at center top by an arrow. | |
| Specialty | Orthopedics |
| Symptoms | Pain and tenderness at the inside of the elbow[1] |
| Risk factors | Repetitive movements (turning the palm down, bending the wrist forwards)[3] |
| Diagnostic method | Based on symptoms[1] |
| Differential diagnosis | Cervical radiculopathy, ulnar collateral ligament injury, osteochondritis dissecans, cubital tunnel syndrome, ulnar neuropathy at the elbow[3][1] |
| Treatment | Altering activity, NSAIDs, physiotherapy, splinting, steroid injections[1] |
| Frequency | Uncommon[3] |
Golfer's elbow, also known as medial epicondylitis, is a tendinopathy of the common flexor tendon.[1] Symptoms include pain and tenderness at the inside of the elbow, which is typically worsened when bending forwards at the wrist against resistance.[1][4] This pain may spread down the forearm towards the wrist and weakened grip may occur.[1] Typically the dominant arm is involved.[1]
It typically occurs due to repetitive movements that involve turning the palm down and bending the wrist forwards; though, occasionally may result following a single injury.[3][1] Groups at particular risk include carpenters, plumbers, golfers, and those who throw overhead.[3][1] Other risks include smoking, obesity, and diabetes.[1] Diagnosis is generally based on symptoms.[1] It is similar to tennis elbow, which affects the outside of the elbow.[3]
Treatment includes altering activity, NSAIDs, and physiotherapy.[1] Splinting the wrist in a slightly bent back position at night or steroid injections may be useful.[1] Rarely surgery may be performed.[1] Outcomes are generally good.[1]
Golfer's elbow is uncommon, being present in less than 1% of people.[3] Onset is generally between 45 and 65 years old.[1] More than 90% of cases are not related to sports.[1] Early descriptions of the condition date to 1882 by Morris who called it "lawn-tennis arm".[5]
Signs and symptoms
Symptoms in include pain at the inside of the elbow.[1]
Causes
The condition is referred to as golfer's elbow or pitcher's elbow due to the same tendon being stressed by repetitive throwing of objects, such as a baseball or football.[1][6][7]
Golfer's elbow appears to occur from repetitive full swings during the period from the top of the backswing to just before ball impact.[1] The full swing motion causes high energy valgus forces during the late cocking (backswing in golf) and acceleration phase (downswing and impact).[1]
It is unknown whether this condition is any more common in labor-related occupations with forceful repetitive activities (such as in construction or plumbing) than it is in the general public.[1]
In adults, the pathophysiology may involve mucoid degeneration (disorganized collagen, increased extra-cellular matrix, and chondroid metaplasia).[8]
Pathophysiology
The tendinopathy results from overload or repetitive use of the arm, causing an injury similar to ulnar collateral ligament injury of the elbow in "pitcher's elbow".[1] The injury is not acute inflammation, but rather is a chronic disorder resulting from overuse of a repetitive arm motion.[1][9] Repetitive activity leads to recurrent microtears within the flexor tendon, with remodeling of the collagen fibers and an increase in the amount of mucoid ground substance.[1] As a result, scar tissue formation and thickening of the tendon lead to reduced collagen strength and pain with repetitive use.[1]
The anterior-medial forearm contains several muscles that flex the wrist and pronate the forearm.[1] These muscles have a common tendinous attachment at the medial epicondyle of the humerus at the elbow joint.[1] The flexor and pronator muscles of the forearm include the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis, all of which originate on the medial epicondyle and are innervated by the median nerve.[1] The flexor carpi ulnaris muscle also inserts on the medial epicondyle and is innervated by the ulnar nerve.[1] Together, these five muscles have a common attachment (an enthesis) on the medial epicondyle of the humerus.[1] The flexor tendon is approximately 3 centimetres (1.2 in) long, crosses the medial aspect of the elbow, and runs parallel to the ulnar collateral ligament.[1]
Diagnosis
Medial epicondylitis is diagnosed based on characteristic pain with activities using strength in wrist flexion and confirmed on examination with discrete point tenderness over the common flexor origin at the medial epicondyle, and pain with resisted wrist flexion and passive wrist extension.[1][9][7][10]
Imaging may be employed, although radiography might show calcifications in the muscle origin. Ultrasound and magnetic resonance imaging can identify the mucoid degeneration, but are not necessary for diagnosis.[1][9][7]
Treatment
Non-specific treatments include:[1][9][7]
- Non-steroidal anti-inflammatory drugs (NSAIDs): ibuprofen, naproxen or aspirin
- Heat or ice
- A counterforce brace or "elbow strap" to reduce strain at the elbow epicondyle, to limit pain provocation and to protect against further damage.
Before anesthetics and steroids are used, conservative treatment with an occupational therapist may be attempted. Before therapy can commence, treatment such as rest, ice, compression and elevation (R.I.C.E.) will typically be used.[1][9][7] This will help to decrease the pain and inflammation; rest will alleviate discomfort because golfer's elbow is an overuse injury. The subject can use a tennis elbow splint for compression. A pad can be placed anteromedially on the proximal forearm.[11] The splint is made in 30–45 degrees of elbow flexion. A daytime elbow pad also may be useful, by limiting additional trauma to the nerve.[12]
Simple analgesic medication has a place, as does more specific treatment with oral anti-inflammatory medications.[1][9][7] These will help control pain and any inflammation.[11] A more invasive treatment is the injection into and around the inflamed and tender area of a glucocorticoid (steroid) agent.[13]
Physical therapy
Therapy includes a variety of exercises for muscle and tendon reconditioning, starting with stretching and gradual strengthening of the flexor-pronator muscles.[9][7][10] Strengthening will slowly begin with isometrics and progresses to eccentric exercises helping to extend the range of motion back to where it once was. After the strengthening exercises, it is common for the subject to ice the area.[11]
- Taping is a way to aid in the treatment of golfer's elbow. It is meant to mimic the skins elasticity, allowing for muscle support without restriction of range of motion. Introducing it has shown effects of improving sensory feedback and the force sense accuracy of patients. Improving force sense accuracy can help with the gripping of objects while improving sensory feedback can help with muscle control and reducing strain. Together, these improvements can enhance overall muscle activation, reduce pain and support the tendon's affected at the elbow. Taping can be used supplementally with other modes of therapy to allow for greater gains.[14]
- Platelet-rich plasma (PRP) While ultrasound-guided PRP injections are increasingly being used, a systemic review found no significant differences in pain relief or functional improvements compared to control treatments for lateral and medial epicondylitis. Patients also reported feeling pain at the PRP injection site. The effectiveness of PRP injections remain uncertain at this point, and more studies are needed. [15]
Surgery
After 6 months if the symptoms do not improve, surgery may be recommended.[1][9][7] Surgical debridement or cleaning of the area is one of the most common treatments.[10] The ulnar nerve may also be decompressed surgically.[11] If the appropriate remediation steps are taken – rest, ice, and rehabilitative exercise and stretching – recovery may follow. Few subjects will need to progress to steroid injection, and less than 10% will require surgical intervention.[11] Arthroscopy is not an option for treating golfer's elbow.[10]
Occurrence
Medial injury of the flexor tendon is estimated to occur in 0.4% of the population.[1] It occurs most often in people ages 45 to 64, is more common in women than in men, and with 75% of cases in the dominant arm.[1]
Risk factors for developing golfer's elbow include improper technique or lack of strength, endurance, or flexibility.[1] Risk factors in people performing manual labor include heavy and excessive repetition, high body mass index, the presence of comorbidities, and high work demands.[1]
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 1.38 1.39 1.40 1.41 1.42 1.43 Kiel, John; Kaiser, Kimberly (27 October 2018), Golfers elbow, StatPearls Publishing, PMID 30085542, archived from the original on 2020-05-15, retrieved 2019-03-12
- ↑ Ebnezar, John; John, Rakesh (31 December 2016). Textbook of Orthopedics. JP Medical Ltd. p. 376. ISBN 978-93-86056-68-9. Retrieved 10 October 2025.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Barco, R; Antuña, SA (August 2017). "Medial elbow pain". EFORT open reviews. 2 (8): 362–371. doi:10.1302/2058-5241.2.160006. PMID 28932488.
- ↑ Millar, NL; Silbernagel, KG; Thorborg, K; Kirwan, PD; Galatz, LM; Abrams, GD; Murrell, GAC; McInnes, IB; Rodeo, SA (7 January 2021). "Tendinopathy". Nature reviews. Disease primers. 7 (1): 1. doi:10.1038/s41572-020-00234-1. PMID 33414454.
- ↑ Graveling, Richard (25 October 2018). Ergonomics and Musculoskeletal Disorders (MSDs) in the Workplace: A Forensic and Epidemiological Analysis. CRC Press. p. PA1998. ISBN 978-1-351-72132-5. Retrieved 10 October 2025.
- ↑ "Pitcher's Elbow – Stanford Sports Medicine – Stanford Medical Outpatient Center". Stanford University Medical Center. Archived from the original on 5 July 2010. Retrieved 9 September 2009.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Wilson, JJ; Best, TM (1 September 2005). "Common overuse tendon problems: A review and recommendations for treatment". American Family Physician. 72 (5): 811–818. PMID 16156339. Archived (PDF) from the original on 29 August 2008. Retrieved 25 March 2025.
- ↑ Bruni, D.; Pierson, S.; Sarwar, F.; Ring, D.; Ramtin, S. (2023). "Are the Pathologic Features of Enthesopathy, Tendinopathy, and Labral and Articular Disc Disease Related to Mucoid Degeneration? A Systematic Review". Clinical Orthopaedics and Related Research. 481 (4): 641–650. doi:10.1097/CORR.0000000000002499. PMC 10013668. PMID 36563131.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Childress MA, Beutler A (April 2013). "Management of chronic tendon injuries". American Family Physician. 87 (7): 486–90. PMID 23547590. Archived from the original on 2025-03-28. Retrieved 2025-03-25.
- ↑ 10.0 10.1 10.2 10.3 Amin, Nirav H.; Kumar, Neil S.; Schickendantz, Mark S. (June 2015). "Medial Epicondylitis: Evaluation and Management". Journal of the American Academy of Orthopaedic Surgeons. 23 (6): 348–355. doi:10.5435/JAAOS-D-14-00145. PMID 26001427. S2CID 31827631.
- ↑ 11.0 11.1 11.2 11.3 11.4 Medial Epicondylitis at eMedicine
- ↑ "Golfers Elbow | Orthopedic Solutions". orthopedicsolutionsokc.com. Archived from the original on 2022-10-07. Retrieved 2025-03-25.
- ↑ Jacobs, J.W.G.; Michels-van Amelsfort, J.M.R. (April 2013). "How to perform local soft-tissue glucocorticoid injections?". Best Practice & Research Clinical Rheumatology. 27 (2): 171–194. doi:10.1016/j.berh.2013.03.003. PMID 23731930.
- ↑ Ghai, Shashank; Ghai, Ishan; Narciss, Susanne (2023-10-20). "Influence of taping on force sense accuracy: a systematic review with between and within group meta-analysis". BMC Sports Science, Medicine & Rehabilitation. 15 (1): 138. doi:10.1186/s13102-023-00740-1. ISSN 2052-1847. PMC 10588111. PMID 37864268.
- ↑ Masiello, Francesca; Pati, Ilaria; Veropalumbo, Eva; Pupella, Simonetta; Cruciani, Mario; De Angelis, Vincenzo (March 2023). "Ultrasound-guided injection of platelet-rich plasma for tendinopathies: a systematic review and meta-analysis". Blood Transfusion = Trasfusione del Sangue. 21 (2): 119–136. doi:10.2450/2022.0087-22. ISSN 2385-2070. PMC 10072988. PMID 36346880.
| Classification | |
|---|---|
| External resources |