Emmonsiosis
| Emmonsiosis | |
|---|---|
| Other names: Emergomycosis[1], Emergomyces infection[2] | |
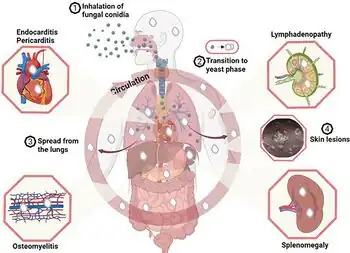 | |
| Effects of Emergomyces infection[3] | |
| Specialty | Infectious diseases[4] |
| Symptoms | Skin rash[4] |
| Causes | Emergomyces, previously under genus Emmonsia[5] |
| Risk factors | HIV, organ transplant, steroid use.[1] |
| Diagnostic method | Skin biopsy, histopathology[1] |
| Differential diagnosis | Histoplasmosis, tuberculosis[6] |
| Treatment | Amphotericin B followed by itraconazole[1][5] |
| Frequency | Rare[1] |
Emmonsiosis, also known as emergomycosis, is a systemic fungal infection that can affect the lungs, generally always affects the skin and can become widespread.[1][4] The lesions in the skin look like small red bumps and patches with a dip, ulcer and dead tissue in the centre.[7]
It is caused by the Emergomyces species, a new fungus, previously classified under the genus Emmonsia.[5] These fungi are found in soil and transmitted by breathing in its spores from the air.[1] Inside the body it converts to yeast-like cells which then cause disease and can invade beyond the lungs.[1] Diagnosis is by skin biopsy, its appearance under the microscope, and culture.[8] It is difficult to distinguish from histoplasmosis and tuberculosis.[6]
Treatment is usually with up to 2 weeks of amphotericin B, following which itraconazole by mouth for around one year.[5] Emmonsiosis can be fatal.[5] The disseminated type is more common in South Africa, particularly in people with HIV.[5]
The disease is named for Chester Wilson Emmons who first described Emmonsia.[9]
Signs and symptoms
Generally, all cases have involvement of the skin.[8] The lesions look like small red bumps and patches with a dip, ulcer and dead tissue in the centre.[7] There may be several lesions and their distribution can be widespread.[1] The lungs may be affected.[5][7]
Cause
It is caused by the Emergomyces species, a novel dimorphic fungus, previously classified under the genus Emmonsia.[5][10] Following a revised taxonomy in 2017 based on DNA sequence analyses, five of these Emmonsia-like fungi have been placed under the separate genus Emergomyces.[5] These include Emergomyces pasteurianus, Emergomyces africanus, Emergomyces canadensis, Emergomyces orientalis and Emergomyces europaeus.[5][11]
Emergomyces africanus was previously known as Emmonsia africanus, which has similar features to Histoplasma spp. and the family of Ajellomycetaceae.[12]
The disease has been observed among people who have a weakened immune system and risk factors include HIV, organ transplant and steroid use.[1][5]
Mechanism
The fungus is found in soil and is released in the air. Transmission is by breathing in fungal spores from the air.[1] Inside the body it converts to yeast-like cells which then cause disease and can invade beyond the lungs.[1] In people with HIV, Emmonsiosis has been associated with Immune reconstitution inflammatory syndrome following initiating antiretroviral treatment.[1]
Diagnosis
Diagnosis is by skin biopsy and its appearance under the microscope.[8]
Differential diagnosis
Generally, it is difficult to distinguish from histoplasmosis.[12] Other conditions that appear similar include tuberculosis,[8] blastomycosis, sporotrichosis, chicken pox, Kaposi's sarcoma and drug reactions.[7]
Treatment
Treatment is usually with up to 2 weeks of amphotericin B, following which itraconazole by mouth for around one year.[5]
Prognosis
It can be fatal.[8]
Epidemiology
The disseminated type is more prevalent in South Africa, particularly in people with HIV.[8]
History
The disease was thought to be a rare condition of the lung.[4] Early cases may have been misdiagnosed as histoplasmosis.[12]
Other animals
The genus Emmonsia can cause adiaspiromycosis, a lung disease in wild animals.[13]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Schwartz, Ilan S.; Govender, Nelesh P.; Sigler, Lynne; Jiang, Yanping; Maphanga, Tsidiso G.; Toplis, Barbra; Botha, Alfred; Dukik, Karolina; Hoving, J. Claire; Muñoz, Jose F.; Hoog, Sybren de; Cuomo, Christina A.; Colebunders, Robert; Kenyon, Chris (19 September 2019). "Emergomyces: The global rise of new dimorphic fungal pathogens". PLOS Pathogens. 15 (9): e1007977. doi:10.1371/journal.ppat.1007977. ISSN 1553-7374. Archived from the original on 6 March 2021. Retrieved 14 March 2022.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ "Orphanet: Emergomycosis". www.orpha.net.
- ↑ Ibe, Chibuike; Mnyambwa, Nicholaus P; Mfinanga, Sayoki G (31 December 2023). "Emergomycosis in Africa: Time to Pay Attention to This Emerging Deadly Fungal Infection". International Journal of General Medicine. 16: 2313–2322. doi:10.2147/IJGM.S403797.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ 4.0 4.1 4.2 4.3 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Archived from the original on 1 August 2018. Retrieved 28 May 2021.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 Samaddar, Arghadip; Sharma, Anuradha (2021). "Emergomycosis, an Emerging Systemic Mycosis in Immunocompromised Patients: Current Trends and Future Prospects". Frontiers in Medicine. 8: 670731. doi:10.3389/fmed.2021.670731. ISSN 2296-858X. PMID 33968970. Archived from the original on 2021-06-04. Retrieved 2021-06-03.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ 6.0 6.1 Proia, Laurie (2020). "28. The dimorphic mycoses". In Spec, Andrej; Escota, Gerome V.; Chrisler, Courtney; Davies, Bethany (eds.). Comprehensive Review of Infectious Diseases. Elsevier. p. 423. ISBN 978-0-323-56866-1. Archived from the original on 2021-08-28. Retrieved 2021-07-12.
- ↑ 7.0 7.1 7.2 7.3 Kutzner, Heinz; Kempf, Werner; Feit, Josef; Sangueza, Omar (2021). "2. Fungal infections". Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses. Hoboken: Wiley Blackwell. p. 102. ISBN 978-1-119-64706-5. Archived from the original on 2021-06-02. Retrieved 2021-05-29.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Schwartz, Ilan S.; Govender, Nelesh P.; Corcoran, Craig; Dlamini, Sipho; Prozesky, Hans; Burton, Rosie; Mendelson, Marc; Taljaard, Jantjie; Lehloenya, Rannakoe; Calligaro, Greg; Colebunders, Robert; Kenyon, Chris (15 September 2015). "Clinical Characteristics, Diagnosis, Management, and Outcomes of Disseminated Emmonsiosis: A Retrospective Case Series" (PDF). Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 61 (6): 1004–1012. doi:10.1093/cid/civ439. ISSN 1537-6591. PMID 26060283. Archived from the original on 14 March 2022. Retrieved 2 June 2021.
- ↑ Henry, Ronnie. "Etymologia: Emmonsia - Volume 23, Number 2—February 2017 - Emerging Infectious Diseases journal - CDC". doi:10.3201/eid2302.et2302. S2CID 5504465. Archived from the original on June 2, 2021. Retrieved June 15, 2021.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Govender, Nelesh P.; Grayson, Wayne (2019). "Emergomycosis (Emergomyces africanus) in Advanced HIV Disease". Dermatopathology. 6 (2): 63–69. doi:10.1159/000495405. ISSN 2296-3529. PMID 31700845. Archived from the original on 2021-08-28. Retrieved 2021-06-03.
- ↑ Jiang, Yanping; Dukik, Karolina; Muñoz, Jose F.; Sigler, Lynne; Schwartz, Ilan S.; Govender, Nelesh P.; Kenyon, Chris; Feng, Peiying; van den Ende, Bert Gerrits; Stielow, J. Benjamin; Stchigel, Alberto M.; Lu, Hongguang; de Hoog, Sybren (1 May 2018). "Phylogeny, ecology and taxonomy of systemic pathogens and their relatives in Ajellomycetaceae (Onygenales): Blastomyces, Emergomyces, Emmonsia, Emmonsiellopsis". Fungal Diversity. 90 (1): 245–291. doi:10.1007/s13225-018-0403-y. ISSN 1878-9129. Archived from the original on 4 June 2021. Retrieved 4 June 2021.
- ↑ 12.0 12.1 12.2 Calonje, J. Eduardo; Grayson, Wayne (2020). "18. Infectious diseases of the skin". In Calonje, J. Eduardo; Brenn, Thomas; Lazar, Alexander J.; Billings, Steven D. (eds.). McKee's Pathology of the Skin, 2 Volume Set (5th ed.). Elsevier. pp. 959–960. ISBN 978-0-7020-6983-3. Archived from the original on 2021-06-02. Retrieved 2021-05-29.
- ↑ Henry, Ronnie Etymologia: Emmonsia Archived 2021-06-02 at the Wayback Machine. Emerging Infectious Diseases. 2017;23(2):348. doi:10.3201/eid2302.et2302.