Lymphatic malformations
| Lymphatic malformation | |
|---|---|
 | |
| Lymphatic malformation of the neck | |
| Specialty | Vascular surgery, interventional radiology, dermatology, plastic surgery |
Lymphatic malformations (LMs) are congenital, benign slow-flow vascular malformations of the lymphatic system characterized by abnormally dilated lymphatic vessels that do not connect properly to the normal lymphatic circulation. These malformations represent developmental anomalies that occur during embryonic lymphatic system formation and are primarily caused by somatic activating mutations in the PIK3CA gene, found in approximately 75-80% of cases.[1]
The umberella term "lymphatic malformation" has replaced older terminology including "lymphangioma," "cystic hygroma," and "lymphangioma circumscriptum."[2] This is because the suffix -ioma imply a relationship to cancer, but these malformations are not cancerous.
Classification
According to the International Society for the Study of Vascular Anomalies (ISSVA), lymphatic malformations are classified as slow-flow vascular malformations (distinguished from vascular tumors which have proliferative endothelial cells) and are divided into three main categories:[3]
Isolated Lymphatic Malformations
- Macrocystic: Contain cysts greater than 2 cm³ in volume
- Microcystic: Contain cysts smaller than 2 cm³ in volume
- Mixed Macro-microcystic: Contain both macrocystic and microcystic components
- Angiokeratoma: Small superficial lesions with lymphatic and vascular components
Complex Lymphatic Malformations
- Generalized Lymphatic Anomaly (GLA): Widespread lymphatic involvement
- Kaposiform Lymphangiomatosis (KLA): Characterized by spindle-shaped lymphatic endothelial cells
- Gorham-Stout Disease (GSD): Progressive bone resorption with lymphatic proliferation
- Central Conducting Lymphatic Anomaly (CCLA): Abnormalities of the central lymphatic system
Lymphedemas
Primary lymphedema:
- Isolated
- Syndromic (including RASopathy-associated)
Secondary lymphedema:
- Acquired due to damage, obstruction, or removal of lymphatic vessels
Epidemiology
The overall incidence of lymphatic malformations ranges from 1 in 6000 to 1 in 16,000, with no predilection for sex or race.[4] However, precise epidemiological data is difficult to establish due to variations in diagnosis, classification systems, and reporting practices across different healthcare systems. Based on these incidence rates, lymphatic malformations are classified as rare diseases.
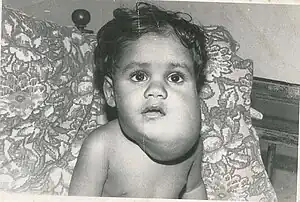
While lymphatic malformations can become evident at any age, most are identified at birth or in early childhood, though some may not be noticed until the teenage years or early adulthood if small or located inside the body. Approximately 75% occur in the lymphatic-rich head and neck region, though they can affect any part of the body including the axilla, mediastinum, buttock, pelvis, and other locations.[5]
Causes
PIK3CA Mutations
The primary cause of lymphatic malformations is now well understood. Somatic activating mutations in the PIK3CA gene are found in approximately 75-80% of lymphatic malformations.[6] These are non-inherited mutations that occur specifically in lymphatic endothelial cells during embryonic development.[7]
The PIK3CA gene encodes a subunit of phosphatidylinositol 3-kinase (PI3K), which regulates cell growth through the PI3K/mTOR pathway. Activating mutations lead to abnormal cell proliferation and lymphatic vessel development.[8] The mutations are specifically localized to the lymphatic endothelial cells lining the malformed vessels, not to surrounding tissues.
Syndromic Associations
Lymphatic malformations may also occur as part of genetic syndromes, including:
- Noonan syndrome
- Turner syndrome
- Down syndrome (trisomy 21)
- Trisomies 13 and 18
Clinical Presentation
Lymphatic malformations typically present as soft, compressible masses that can vary significantly in size and location. The clinical presentation depends on the type and location:
Microcystic lymphatic malformations (formerly lymphangioma circumscriptum):
- Appear as clusters of small, translucent vesicles on the skin surface
- Range in color from pink to dark red
- May leak clear lymphatic fluid or occasionally bleed when ruptured
Macrocystic lymphatic malformations (formerly cystic hygroma):
- Present as larger, deeper masses with a soft, doughy consistency
- Commonly occur in the neck (75%), axilla, or groin
- Can cause compression symptoms if large
- May fluctuate in size
Mixed malformations:
- Display characteristics of both microcystic and macrocystic types
- Can be more complex and challenging to treat
Complications
While lymphatic malformations are benign (non-cancerous), they can cause significant symptoms and complications that substantially impact quality of life:
- Recurrent infections: Cellulitis and lymphangitis can cause severe pain, swelling, and systemic illness. These infections may be recurrent and difficult to treat, requiring frequent hospitalizations and long-term antibiotic therapy.
- Chronic pain and discomfort: Ongoing pain from tissue distension, pressure effects, and recurrent infections.
- Functional impairment: Depending on location and size, malformations can interfere with movement, eating, speaking, or other essential functions.
- Psychological and social impact: Visible malformations can affect self-esteem, social interactions, and mental health.
- Bleeding: Trauma to superficial vessels can cause bleeding.
- Compression effects: Large malformations can compress vital structures, causing respiratory distress, swallowing difficulties, or neurological symptoms.
- Lymph leakage: Chronic drainage can lead to skin breakdown, secondary infections, and social difficulties.
- Overgrowth: Progressive enlargement of affected tissues and bones can cause asymmetry and functional problems.
Treatment
Treatment approach depends on the size, location, severity of symptoms, and impact on quality of life and function. The goal is not merely cosmetic improvement, but comprehensive management of symptoms, prevention of complications, and optimization of quality of life. Treatment decisions should involve multidisciplinary teams familiar with vascular anomalies, as these conditions are often poorly understood by general medical practitioners.
Surgical Management
Complete surgical excision remains the treatment of choice when feasible, offering the best chance for cure. However, complete removal may not be possible without sacrificing important structures, particularly for extensive microcystic malformations.
Sclerotherapy
Sclerotherapy has become a primary treatment modality, particularly for macrocystic malformations. Various sclerosing agents are used:
Sclerosing agents work by damaging the endothelial lining of the abnormal lymphatic vessels.
Medical Therapy
Sirolimus (rapamycin): An mTOR inhibitor that has emerged as an important medical treatment option. It can decrease the size of lymphatic malformations, reduce symptoms, and improve quality of life, particularly in patients with PIK3CA mutations affecting the PI3K/mTOR pathway.[9] Sirolimus is a macrolide compound which has immunosuppressant and antiproliferative functions in humans. It inhibits activation of T cells and B cells by reducing their sensitivity to interleukin-2 (IL-2) through mTOR inhibition.[10]
Targeted therapies: Research is ongoing into therapies specifically targeting PIK3CA-mutated cells.
Other Treatments
- Laser therapy: Pulsed dye laser may be effective for superficial microcystic lesions
- Supportive care: Compression garments, wound care for leaking lesions
Prognosis
The prognosis for lymphatic malformations is generally good, as they are benign lesions with no malignant potential under normal circumstances. Factors affecting prognosis include:
- Location: Head and neck lesions may cause more functional problems
- Size and extent: Larger, more extensive lesions are more challenging to treat
- Type: Macrocystic lesions generally respond better to sclerotherapy
- Associated syndromes: May complicate management and prognosis
Complete cure is possible with total surgical excision, but recurrence can occur if residual tissue remains. Medical therapies like sirolimus can provide significant symptom improvement and size reduction but typically require ongoing treatment.
History
The understanding and classification of lymphatic malformations has evolved significantly:
- 1828: Redenbacher first described lymphangioma lesions.[11]
- 1843: Wernher described the condition in his 1843 publication, Die angeborenen Kysten-hygrome und die ihnen verwandten Geschwülste (Congenital cystic hygromas and related tumors).[12]
- 1965: Bill and Summer proposed that cystic hygromas and lymphangiomas represent variations of a single entity.
- 1976: Whimster studied the pathogenesis of lymphangioma circumscriptum, providing insights into the developmental basis.[13]
- 2014-2015: Discovery of PIK3CA mutations as the primary cause of lymphatic malformations, revolutionizing understanding of pathogenesis.
- 2018: ISSVA classification update standardizing terminology to "lymphatic malformation".[14]
References
- ↑ Mäkinen, Taija; Boon, Laurence M.; Vikkula, Miikka; Alitalo, Kari (2021-06-25). "Lymphatic Malformations: Genetics, Mechanisms and Therapeutic Strategies". Circulation Research. 129 (1): 136–154. doi:10.1161/CIRCRESAHA.121.318142. hdl:2078.1/248427. PMID 34166072.
- ↑ "Lymphatic Malformations - Symptoms, Causes, Treatment | NORD". Retrieved 2025-09-09.
- ↑ "Classification | International Society for the Study of Vascular Anomalies". www.issva.org. Retrieved 2025-09-09.
- ↑ Lee, Su Yeon; Loll, Emma Grace; Hassan, Abd-Elrahman Said; Cheng, Mingyu; Wang, Aijun; Farmer, Diana Lee (2022-02-08). "Genetic and Molecular Determinants of Lymphatic Malformations: Potential Targets for Therapy". Journal of Developmental Biology. 10 (1): 11. doi:10.3390/jdb10010011. ISSN 2221-3759. PMC 8883961. PMID 35225964.
- ↑ Beech, A. N.; Farrier, J. N. (2016). "An Interesting Association of Cystic Hygroma of the Neck and Lymphangioma Causing a Paediatric Swollen Tongue". Case Reports in Pediatrics. 2016 7930945. doi:10.1155/2016/7930945. ISSN 2090-6803. PMC 4812285. PMID 27069707.
- ↑ Luks, Valerie L.; Kamitaki, Nolan; Vivero, Matthew P.; Uller, Wibke; Rab, Rashed; Bovée, Judith V. M. G.; Rialon, Kristy L.; Guevara, Carlos J.; Alomari, Ahmad I.; Greene, Arin K.; Fishman, Steven J.; Kozakewich, Harry P. W.; Maclellan, Reid A.; Mulliken, John B.; Rahbar, Reza (April 2015). "Lymphatic and other vascular malformative/overgrowth disorders are caused by somatic mutations in PIK3CA". The Journal of Pediatrics. 166 (4): 1048–1054.e1–5. doi:10.1016/j.jpeds.2014.12.069. ISSN 1097-6833. PMC 4498659. PMID 25681199.
- ↑ Blesinger, Hannah; Kaulfuß, Silke; Aung, Thiha; Schwoch, Sonja; Prantl, Lukas; Rößler, Jochen; Wilting, Jörg; Becker, Jürgen (2018-07-09). "PIK3CA mutations are specifically localized to lymphatic endothelial cells of lymphatic malformations". PLOS ONE. 13 (7) e0200343. Bibcode:2018PLoSO..1300343B. doi:10.1371/journal.pone.0200343. ISSN 1932-6203. PMC 6037383. PMID 29985963.
- ↑ Osborn, Alexander J.; Dickie, Peter; Neilson, Derek E.; Glaser, Kathryn; Lynch, Kaari A.; Gupta, Anita; Dickie, Belinda Hsi (2015-02-15). "Activating PIK3CA alleles and lymphangiogenic phenotype of lymphatic endothelial cells isolated from lymphatic malformations". Human Molecular Genetics. 24 (4): 926–938. doi:10.1093/hmg/ddu505. ISSN 1460-2083. PMID 25292196.
- ↑ Wang, Jialu; Meng, Yiran; Zhang, Xuexi; Li, Yanzhen; Sun, Nian; Liu, Qiaoyin; Peng, Yun; Cheng, Xiaoling; Liu, Yuanhu; Liu, Zhiyong; Liu, Yuwei; Zhang, Ge; Ni, Xin; Wang, Shengcai (2025-07-01). "A real-world study of sirolimus in the treatment of pediatric head and neck lymphatic malformations". Journal of Vascular Surgery: Venous and Lymphatic Disorders. 13 (4) 102230. doi:10.1016/j.jvsv.2025.102230. ISSN 2213-333X. PMC 12433909.
- ↑ Sehgal, S. N. (May 2003). "Sirolimus: its discovery, biological properties, and mechanism of action". Transplantation Proceedings. 35 (3 Suppl): 7S – 14S. doi:10.1016/s0041-1345(03)00211-2. ISSN 0041-1345. PMID 12742462.
- ↑ Sharma, J. V. Pranav; Kazi, Farah Naaz (March 2021). "Cystic lymphangioma in adult-a rare case scenario or a misdiagnosis?". Journal of Surgical Case Reports. 2021 (3) rjab062. doi:10.1093/jscr/rjab062. ISSN 2042-8812. PMC 7958348. PMID 33747431.
- ↑ Colangeli, Walter; Facchini, Valerio; Kapitonov, Aleksandr; Zappalà, Marta; Bozza, Fabrizio; Becelli, Roberto (July 2020). "Cystic lymphangioma in adult: a case report and a review of the literature". Journal of Surgical Case Reports. 2020 (7) rjaa179. doi:10.1093/jscr/rjaa179. ISSN 2042-8812. PMC 7394139. PMID 32760485.
- ↑ Whimster, I.w. (1976). "The pathology of lymphangioma circumscriptum". British Journal of Dermatology. 94 (5): 473–486. doi:10.1111/j.1365-2133.1976.tb05134.x. ISSN 1365-2133.
- ↑ "Classification | International Society for the Study of Vascular Anomalies". www.issva.org. Retrieved 2025-09-10.