Fixed drug reaction
| Fixed drug reaction | |
|---|---|
| Other names: Fixed drug eruption | |
.jpg) | |
| Fixed drug reaction | |
| Specialty | Dermatology |
| Symptoms | One or several red/purple skin patches in same location every time a particular drug is taken,[1] typically on face, lips, groin[2] |
| Usual onset | Around 2 hours after taking drug,[1] can be 2 weeks[3] |
| Causes | Type IV hypersensitivity,[4] antibiotics, non-steroidal anti-inflammatory drugs[4] |
| Diagnostic method | History, visualisation, skin biopsy, oral challenge test, patch test[4] |
| Differential diagnosis | Insect bite reaction, bullous pemphigoid, erythema multiforme, Stevens-Johnson syndrome, herpes simplex, aphthous ulcer[4] |
| Treatment | Identify and stop causative drug, topical corticosteroid[4] |
| Frequency | Common, males=females, age 35-60 years[3] |
A fixed drug reaction is a rash that appears in the same fixed location every time a particular drug is taken.[1] It is typically a solitary well-defined, roundish red or purplish patch.[1][2] There may however be several which can be scattered or generalized, and there may be blisters, vesicles, erosions or ulcers.[3] It can be itchy and painful and often leaves a dark mark after healing.[4] Common sites include face, lips, groin, hands, feet, eyelids, anogenital areas, tongue and hard palate.[2][4]
It is a delayed type IV hypersensitivity, usually caused by antibiotics and non-steroidal anti-inflammatory drugs.[4] A typical time from taking the drug to noticing the rash is around 2 hours,[1] but can be 2 weeks.[3] Diagnosis is by history and visualisation of the rash.[3] It may require a skin biopsy, oral challenge test with a low dose of the suspected drug or a patch test.[4] The first epiode may be mistaken for an insect bite reaction or bullous pemphigoid.[4] Other differentials include erythema multiforme, Stevens-Johnson syndrome, herpes simplex or aphthous ulcer.[4]
Treatment includes identifying and stopping the causative drug and considering applying topical corticosteroid.[4]
They are common.[1] Males are affected equally to females.[3] The most likely age group is 35 to 60 years old.[3] It was first described in 1889 and the term was coined by Brocq in 1894.[3]
Signs and symptoms
It generally looks like a solitary or a few well-defined, roundish red or purplish patches which may blister.[4] It can be itchy and painful and often leaves a mark after healing.[4] The lips, genitals, and hands are often involved. The affected person feels otherwise well.[4] Common sites include hands, feet, eyelids, anogenital areas, lips, tongue and hard palate.[4] These sites may be the location of previous trauma such as an insect bite, blood test or burn.[4]
-
.jpg) Fixed drug reaction (targeted)
Fixed drug reaction (targeted) -
.jpg) Fixed drug reaction (pigmented) on lip
Fixed drug reaction (pigmented) on lip -
 Fixed drug reaction on hard palate
Fixed drug reaction on hard palate -
 Fixed drug reaction (lips and penis)
Fixed drug reaction (lips and penis) -
 Fixed drug reactio groin (erosions)
Fixed drug reactio groin (erosions) -
.jpg) Fixed drug reaction to cotrimoxazole
Fixed drug reaction to cotrimoxazole
Causes
It is a delayed type IV hypersensitivity, usually caused by antibiotics and non-steroidal anti-inflammatory drugs.[4] Medications inducing fixed drug reactions are usually those taken intermittently.[1] Medications that are commonly implicated as a cause of fixed drug reactions include the following:
Anti-microbials
- Amoxicillin[3]
- Ciprofloxacin
- Clarithromycin
- Cotrimoxazole(Trimethoprim/sulfamethoxazole)[3]
- Doxycycline[3]
- Fluconazole[4]
- Nystatin[2]
- Levofloxacin[3]
- Trimethoprim[3]
- Quinine[4]
Painkillers
Anti-hypertensive medications
Anti-epileptic drugs
Other
Vaccines
- Influenza vaccine[3]
Foods
Diagnosis
Diagnosis is by history and visualisation of the rash.[3] It may require a skin biopsy, oral challenge test with a low dose of the suspected drug or a patch test.[4]
Tests
-
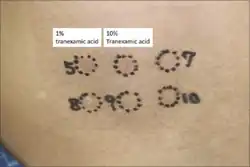 Patch test to tranexamic acid
Patch test to tranexamic acid -
 Patch test to anti-histamines
Patch test to anti-histamines -
.png) A. FDR, B. 30 min after oral challenge test
A. FDR, B. 30 min after oral challenge test
Histopathology
Histopathology show distinct changes in vacuoles and Civatte bodies in all levels of the epidermis.[2] The is melanin incontinence and neutrophils and eosinophils.[2]
-
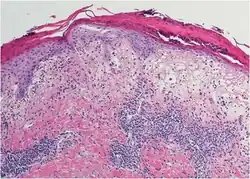 Melanin incontinence
Melanin incontinence -
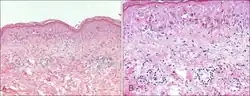 Basal vacuolation
Basal vacuolation
Treatment
Treatment includes identifying and stopping the causative drug and considering applying topical corticosteroid.[4]
Epidemiology
Fixed drug reaction is common.[1] Males are affected equally to females.[3] The most likely age group is 35 to 60 years old.[3]
History
The condition was first described in 1889 and the term was coined by Brocq in 1894.[3]
See also
- List of cutaneous conditions
- List of human leukocyte antigen alleles associated with cutaneous conditions
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "6. Contact dermatitis and drug eruptions". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Elsevier. pp. 120–121. ISBN 978-0-323-54753-6. Archived from the original on 2021-10-16. Retrieved 2021-10-15.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Johnstone, Ronald B. (2017). "3. Lichenoid reaction pattern". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 41. ISBN 978-0-7020-6830-0. Archived from the original on 2021-05-25. Retrieved 2021-10-16.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 Anderson, Hannah J.; Lee, Jason B. (September 2021). "A Review of Fixed Drug Eruption with a Special Focus on Generalized Bullous Fixed Drug Eruption". Medicina. 57 (9): 925. doi:10.3390/medicina57090925. Archived from the original on 2021-10-17. Retrieved 2021-10-16.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 4.33 4.34 4.35 4.36 4.37 4.38 4.39 4.40 4.41 "Fixed drug eruption | DermNet NZ". dermnetnz.org. Archived from the original on 13 August 2021. Retrieved 16 October 2021.
External links
| Classification |
|---|