Vernal keratoconjunctivitis
| Vernal keratoconjunctivitis | |
|---|---|
| Other names: Spring catarrh; warm weather conjunctivitis; spring ophthalmia[1] | |
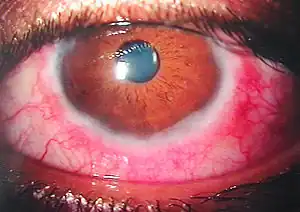 | |
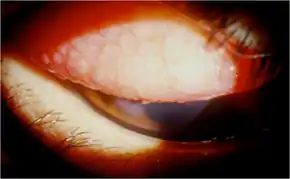
| Some of the cornea and conjunctiva findings in vernal conjunctivitis | |
| Specialty | Ophthalmology |
| Symptoms | Eye itching, eye pain, eye redness, sensitivity to light, white discharge, increased tears[2][1] |
| Complications | Corneal ulcers, cataracts[2] |
| Usual onset | 5 to 10 years old[3] |
| Duration | Long-term[1] |
| Causes | Allergic reaction to airborne allergens[2][1] |
| Risk factors | Personal or family history of atopic diseases[1] |
| Diagnostic method | Based on symptoms[2] |
| Differential diagnosis | Viral conjunctivitis, other types of allergic conjunctivitis[1][4] |
| Treatment | Avoid triggers[1] |
| Medication | Antihistamines, mast cell stabilizer, steroid, cyclosporine, tacrolimus[2][1] |
| Prognosis | Generally resolves with age[4][1] |
| Frequency | 1 to 13 per 100,000 (Western World); Up to 37% (Africa)[4] |
Vernal keratoconjunctivitis (VKC) is a condition that affects the cornea and conjunctiva of both eyes.[2] Symptoms may include eye itching, eye pain, eye redness, sensitivity to light, white discharge, and increased tears.[2][1] Complications may include corneal ulcers and cataracts.[2]
It is a form of allergic reaction to airborne allergens.[2][1] Often there is a personal or family history of atopic diseases.[1] It does not spread between people.[1] Diagnosis is generally based on symptoms.[2] Occationally testing the conjunctiva for eosinophils may be carried out.[1] It is a type of keratoconjunctivitis.[5]
Those affected should avoid triggers.[1] Treatment generally involves some combination of antihistamines, mast cell stabilizers, steroids, cyclosporine, or tacrolimus eye drops.[2][1] Steroids should only be used in severe disease due to associated side effects.[1] Artificial tears or a cold cloth may also be used.[1] Occationally surgery is needed to manage complications.[2] Outcomes are generally good.[6]
Vernal keratoconjunctivitis affects about 1 to 13 per 100,000 people in the Western World; though rates may be as high as 37% in parts of Africa.[4] Onset is generally in childhood and it resolves in 90% with age.[4][1] Males are more commonly affected than females.[1] It is generally long-term, with reoccurances or worsening in the springtime.[1] Those close to the equator are more commonly affected.[2] The condition was first described in 1846 by Arlt.[6]
Sign and symptoms
VKC is characterised by marked burning and itchy sensations which may be intolerable and accentuates when patient comes in a warm humid atmosphere. Associated symptoms include mild photophobia in case of corneal involvement, lacrimation, stringy discharge and heaviness of eyelids.
It can be described in three clinical forms (Cameron Classification):[7]
- Palpebral form- Usually upper tarsal conjunctiva of both the eyes is involved. Typical lesion is characterized by the presence of hard, flat-topped papillae arranged in cobblestone or pavement stone fashion. In severe cases papillae undergo hypertrophy to produce cauliflower-like excrescences of 'giant papillae'.
- Bulbar form- It is characterised by dusky red triangular congestion of bulbar conjunctiva in palpebral area, gelatinous thickened accumulation of tissue around limbus and presence of discrete whitish raised dots along the limbus (Tranta's spots).
- Mixed form- Shows the features of both palpebral and bulbar types.
Cause
VKC is thought to be an allergic disorder in which IgE mediated mechanism play a role. Such patients often give family history of other atopic diseases such as hay fever, asthma or eczema, and their peripheral blood shows eosinophilia and increased serum IgE levels.
Risk factors
- Age and sex – 4–20 years; more common in boys than girls.
- Season – More common in summer. Hence, the name Spring catarrh is a misnomer. Recently it is being labelled as Warm weather conjunctivitis.
- Climate – More prevalent in the tropics. VKC cases are mostly seen in hot months of summer, therefore, more suitable term for this condition is "summer catarrh" Ref.[8]
Pathology
- Conjunctival epithelium undergoes hyperplasia and sends downward projection into sub-epithelial tissue.
- Adenoid layer shows marked cellular infiltration by eosinophils, lymphocytes, plasma cells and histiocytes.
- Fibrous layer show proliferation which later undergoes hyaline changes.
- Conjunctival vessels also show proliferation, increased permeability and vasodilation.
Diagnosis
Types
Corneal involvement in VKC may be primary or secondary due to extension of limbal lesions. Vernal keratopathy includes 5 types of lesions.
- Punctuate epithelial keratitis.
- Ulcerative vernal keratitis (shield ulceration).
- Vernal corneal plaques.
- Subepithelial scarring.
- Pseudogerontoxon.
Classification
Based on severity there are four grades:[9]
- Grade 0 - Absence of symptoms
- Grade 1 Mild - Symptoms but no corneal involvement
- Grade 2 Moderate - Symptoms with photophobia but no corneal involvement
- Grade 3 Severe - Symptoms, photophobia, mild to moderate SPK's OR with Diffuse SPK or corneal ulcer
Treatment
- Local therapy- Topical steroids are effective. Commonly used solutions are of fluorometholone, medrysone, betamethasone or dexamethasone. Mast cell stabilizers such as sodium cromoglycate (2%) drops 4–5 times a day are quite effective in controlling VKC, especially atopic ones. Azelastine eyedrops are also effective. Topical antihistamines can be used. Acetyl cysteine (0.5%) used topically has mucolytic properties and is useful in the treatment of early plaque formation. Topical Cyclosporine is reserved for unresponsive cases.
- Systemic therapy- Oral antihistamines and oral steroids for severe cases.
- Treatment of large papillae- Cryo application, surgical excision or supratarsal application of long-acting steroids.
- General measures include use of dark goggles to prevent photophobia, cold compresses and ice pack for soothing effects, change of place from hot to cold areas.
- Desensitization has also been tried without much rewarding results.
- Treatment of vernal keratopathy- Punctuate epithelial keratitis require no extra treatment except that instillation of steroids should be increased. Large vernal plaque requires surgical excision. Ulcerative vernal keratitis require surgical treatment in the form of debridement, superficial keratectomy, excimer laser therapeutic keratectomy, as well as amniotic membrane transplantation to enhance re-epithelialisation.
- Treatment with tacrolimus ointment (0.1%) used topically twice daily is showing encouraging results.
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 "Vernal Keratonconjunctivitis - Symptoms, Causes, Treatment | NORD". rarediseases.org. NORD. Archived from the original on 1 March 2025. Retrieved 2 March 2025.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Bruschi, G; Ghiglioni, DG; Cozzi, L; Osnaghi, S; Viola, F; Marchisio, P (August 2023). "Vernal Keratoconjunctivitis: A Systematic Review". Clinical reviews in allergy & immunology. 65 (2): 277–329. doi:10.1007/s12016-023-08970-4. PMID 37658939.
- ↑ Baab, S; Le, PH; Gurnani, B; Kinzer, EE (January 2025). "Allergic Conjunctivitis". StatPearls. PMID 28846256.
- ↑ 4.0 4.1 4.2 4.3 4.4 Kaur, K; Gurnani, B (January 2025). "Vernal Keratoconjunctivitis". StatPearls. PMID 35015458.
- ↑ Burrow, Michael K.; Patel, Bhupendra C. (2022). "Keratoconjunctivitis". StatPearls. StatPearls Publishing. PMID 31194419.
- ↑ 6.0 6.1 "Vernal Keratoconjunctivitis - EyeWiki". eyewiki.org. Archived from the original on 10 October 2024. Retrieved 2 March 2025.
- ↑ Cameron, J. A. (June 1995). "Shield ulcers and plaques of the cornea in vernal keratoconjunctivitis". Ophthalmology. 102 (6): 985–993. doi:10.1016/s0161-6420(95)30925-6. ISSN 0161-6420. PMID 7777308.
- ↑ Shah, Syed Imtiaz Ali (2014). Concise Ophthalmology (4th ed.). Paramount. p. 31. ISBN 978-969-637-001-7.
- ↑ S Gokhale, Nikhil (2015-06-27). "Vernal Keratoconjunctivitis Grading System and Step Ladder Management Approach". Delhi Journal of Ophthalmology. 25 (2): 85–89. doi:10.7869/djo.84.
External links
| Classification | |
|---|---|
| External resources |
|