Paraphimosis
| Paraphimosis | |
|---|---|
 | |
| Paraphimosis with arrow pointing to the location of the constricting band created by the foreskin | |
| Pronunciation | |
| Specialty | Emergency medicine, urology |
| Symptoms | Pain and swelling of the tip of the penis[3] |
| Complications | Gangrene of the glans penis[3] |
| Causes | Improper handling or piercing the foreskin[3] |
| Risk factors | Uncircumcised, phimosis[4][5] |
| Diagnostic method | Based on examination[6] |
| Differential diagnosis | Balanitis, penile fracture, hair tourniquet[4] |
| Prevention | Returning the foreskin to its normal position[4] |
| Treatment | Reducing swelling followed by manual reduction, dorsal slit[3] |
| Prognosis | Good with treatment[4] |
| Frequency | Relatively common[4] |
Paraphimosis is when the foreskin becomes trapped above the glans penis resulting in reduced blood return.[3][6] Symptoms often include significant pain and swelling.[3] Occasionally people may be unable to urinate.[3] If this persists gangrene can result.[3]
It only occurs in the partially or uncircumcised.[4] The cause is generally failure to return the foreskin to its normal position, such as after placing a urinary catheter or sexual activity.[3][5] It may also occur following piercing or overly forceful cleaning in a child.[3][6] Diagnosis is based on examination.[6] Prevention involves returning the foreskin to its normal position.[4]
It is an emergency.[3] Management involves reducing swelling and pushing the glans through the stricture.[3] Swelling may be reduced by applying ice, sugar, and manual pressure.[3] Removal of the urinary catheter is generally required.[3] Pain may be reduced with a nerve block, topical lidocaine, or morphine.[3] If other measures are not effective, a cut maybe required.[3]
Paraphimosis is relatively common, represents about 0.2% of foreskin problems in uncircumcised children.[4] It most commonly affects the young and the old.[7] After it has been reduced, the foreskin should not be retracted for a week.[4] Long-term prevention of recurrence is by circumcision or a dorsal slit.[4] The condition has been described since at least 1,200 BC, with the current name coming into use in 100 CE.[8]
Signs and symptoms

Symptoms often include pain and swelling.[3] Occasionally people may be unable to urinate.[3] If this persists gangrene can result.[3]
Causes
Paraphimosis is usually caused by medical professionals (iatrogenic) or parents who handle the foreskin improperly.[9][3] The foreskin may be retracted during penile examination, penile cleaning, urethral catheterization, or cystoscopy; if the foreskin is left retracted for a long period, some of the foreskin tissue may become oedematous (swollen with fluid), which makes subsequent reduction of the foreskin difficult.
Prevention
Paraphimosis can be avoided by bringing the foreskin back into its normal, forward, non-retracted position after retraction is no longer necessary (for instance, after cleaning the glans penis or placing a Foley catheter). Phimosis (both pathologic and normal childhood physiologic forms) is a risk factor for paraphimosis;[10] physiologic phimosis resolves naturally as a child matures, but it may be advisable to treat pathologic phimosis via long-term stretching or elective surgical techniques (such as preputioplasty to loosen the preputial orifice or circumcision to amputate the foreskin tissue partially or completely).
The foreskin responds to the application of tension to cause expansion by creating new skin cells though the process of mitosis. The tissue expansion is permanent. Non-surgical stretching of the foreskin may be used to widen a narrow, non-retractable foreskin.[11] Stretching may be combined with the use of a corticosteroid cream.[12][13] Beaugé recommends manual stretching for young males in preference to circumcision as a treatment for non-retractile foreskin because of the preservation of sexual sensation.[14]
Treatment
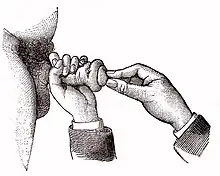
Paraphimosis can often be effectively treated by manual manipulation of the swollen foreskin tissue. This involves compressing the glans penis and moving the foreskin back to its normal position, perhaps with the aid of a lubricant, cold compression, and local anesthesia as necessary. If this fails, the tight edematous band of tissue can be relieved surgically with a dorsal slit,[9][3] or a circumcision.[15][16][17][18][19] An alternative method, the Dundee technique, entails placing multiple punctures in the swollen foreskin with a fine needle, and then expressing the edema fluid by manual pressure.[16] Treatment by circumcision may be elected as a last resort.[20] Other experts recommend delaying elective circumcision until after paraphimosis has been resolved.[9] A non-invasive method is the application of granulated sugar to induce transfer of the hypotonic fluid out of the edematous tissue towards the wet sugar via osmotic gradient, to reduce swelling and enabling manual reduction.[3]
References
- ↑ OED 2nd edition, 1989 as /ˌpærəfaɪˈməʊsɪs/.
- ↑ Entry "paraphimosis" in Merriam-Webster Online Dictionary Archived 2017-09-22 at the Wayback Machine.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 Choe JM (December 2000). "Paraphimosis: current treatment options". American Family Physician. 62 (12): 2623–6, 2628. PMID 11142469. Archived from the original on 2011-08-07. Retrieved 2024-09-19. Archived 2011-08-07 at the Wayback Machine
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 Bragg, BN; Kong, EL; Leslie, SW (January 2025). "Paraphimosis". StatPearls. PMID 29083645. Archived from the original on 2024-12-14. Retrieved 2024-09-19. Archived 2024-12-14 at the Wayback Machine
- ↑ 5.0 5.1 Fahmy, Mohamed A. Baky (6 March 2020). Normal and Abnormal Prepuce. Springer Nature. p. 185. ISBN 978-3-030-37621-5. Archived from the original on 24 April 2025. Retrieved 27 March 2025.
- ↑ 6.0 6.1 6.2 6.3 Manjunath, AS; Hofer, MD (March 2018). "Urologic Emergencies". The Medical clinics of North America. 102 (2): 373–385. doi:10.1016/j.mcna.2017.10.013. PMID 29406065.
- ↑ Offenbacher, J; Barbera, A (November 2019). "Penile Emergencies". Emergency medicine clinics of North America. 37 (4): 583–592. doi:10.1016/j.emc.2019.07.001. PMID 31563196.
- ↑ Fahmy, Mohamed A. Baky (6 March 2020). Normal and Abnormal Prepuce. Springer Nature. p. 180. ISBN 978-3-030-37621-5. Archived from the original on 24 April 2025. Retrieved 27 March 2025.
- ↑ 9.0 9.1 9.2 Donohoe JM, Burnette JO, Brown JA (October 7, 2009). "Paraphimosis". eMedicine. Archived from the original on October 25, 2022. Retrieved September 19, 2024.
Patients with severe paraphimosis that proves refractory to conservative therapy will require a bedside emergency dorsal slit procedure to save the penis. A formal circumcision can be performed in the operating room at a later date... At a later date, a formal circumcision can be performed as an outpatient procedure.
Archived October 25, 2022, at the Wayback Machine - ↑ Ghory HZ, Sharma R (April 28, 2010). "Phimosis and Paraphimosis". eMedicine. Archived from the original on November 3, 2022. Retrieved September 19, 2024.
Patients with phimosis, both physiologic and pathologic, are at risk for developing paraphimosis when the foreskin is forcibly retracted past the glans and/or the patient or caretaker forgets to replace the foreskin after retraction.
Archived November 3, 2022, at the Wayback Machine - ↑ Dunn HP (December 1989). "Non-surgical management of phimosis". The Australian and New Zealand Journal of Surgery. 59 (12): 963. doi:10.1111/j.1445-2197.1989.tb07640.x. PMID 2597103.
- ↑ Zampieri N, Corroppolo M, Camoglio FS, Giacomello L, Ottolenghi A (November 2005). "Phimosis: stretching methods with or without application of topical steroids?". The Journal of Pediatrics. 147 (5): 705–6. doi:10.1016/j.jpeds.2005.07.017. PMID 16291369. S2CID 29301071.
- ↑ Ghysel C, Vander Eeckt K, Bogaert GA (2009). "Long-term efficiency of skin stretching and a topical corticoid cream application for unretractable foreskin and phimosis in prepubertal boys". Urologia Internationalis. 82 (1): 81–8. doi:10.1159/000176031. PMID 19172103. S2CID 5287988.
- ↑ Beaugé M (1997). "The causes of adolescent phimosis". Br J Sex Med (September–October): 26.
- ↑ Santucci RA, Terlecki RP (April 15, 2009). "Phimosis, Adult Circumcision, and Buried Penis". eMedicine. Archived from the original on March 3, 2025. Retrieved September 19, 2024.
Reduction of the foreskin under sedation is almost always possible. However, in some situations, a dorsal slit or circumcision is required
Archived March 3, 2025, at the Wayback Machine - ↑ 16.0 16.1 to be 5 Reynard JM, Barua JM (May 1999). "Reduction of paraphimosis the simple way - the Dundee technique". BJU International. 83 (7): 859–60. doi:10.1046/j.1464-410x.1999.00119.x. PMID 10368214. S2CID 5133709. Archived from the original on 2013-01-05. Archived 2013-01-05 at archive.today
- ↑ Surgical care at the district hospital. World Health Organization. 2003. pp. 9–10. ISBN 92-4-154575-5.
- ↑ Stead LG, Stead SW, Kaufman MS (2006). First Aid for the Emergency Medicine Clerkship. Mcgraw-hill. p. 231. ISBN 0-07-144873-X.
- ↑ Zderic S, Platcher N, Kirk J (2008). Pediatric Urology for the Primary Care Provider. SLACK Incorporated. p. 80. ISBN 978-1-55642-785-5.
- ↑ Ghory HZ, Sharma R (April 28, 2010). "Phimosis and Paraphimosis". eMedicine. Archived from the original on November 24, 2010. Retrieved September 19, 2024. Archived November 24, 2010, at the Wayback Machine
External links
| Classification | |
|---|---|
| External resources |